In this section we have collated articles about the Mental Health Commissioners, Mental Health Trusts and Private hospitals operating in Greater Manchester. The two Trusts are the Greater Manchester Mental Health Foundation Trust and Pennine Care NHS Foundation Trust, the Commissioner is the Greater Manchester Integrated Care Partnership. we have been collating news items since December 2020 and there are now 176 summaries of articles (November 2024).
Our intention is to identify issues and concerns across the services and we do this through monitoring media coverage of mental health services in our City Region.
As you will read below, there is growing evidence of systemic problems that have led to tragic outcomes. (Between April and July 2022 alone there were 12 press reports of Inquests and Court cases involving GMMHT and Pennine Trust).
If you have any information that you think we should know about and that we can share here please let us know.
Click on title for full story
June 2025
Bury MP calls for ‘urgent’ action around mental health wards
A healthcare watchdog carried out an inspection of mental health wards for older people in Greater Manchester after receiving “concerning information” from whistleblowers. Pennine Care NHS Foundation Trust provides mental health services across Greater Manchester, including units at Fairfield General Hospital, Birch Hill Hospital and Royal Oldham Hospital. It was assessed by the Quality Care Commission (CQC) in November last year in response to “concerning information” received about several mental health wards from complaints, whistleblowing concerns and notifications from the trust. The assessment included onsite inspections of all nine of the trust’s wards. The report, which was published in May, found five breaches of regulations and highlighted concerns around staffing, patient care and training. Inspectors found that patients did not always receive “sufficient person-centred support to make their own decisions”.
The report said that patients who were unable to clearly communicate their needs verbally “did not have communication care plans or any planned individualised support to support them in making and communicating decisions about their care”. For patients who might have impaired mental capacity, staff “did not always assess and record capacity to consent appropriately”. It added that relatives and carers “mostly gave positive feedback” but that some reported that they were “only allowed an hour with their relatives”. Inspectors found that it was “not possible” to identify the proportion of staff on each ward who had completed Mental Health Act awareness training or how up to date this was due to it not being compulsory.
The service “did not have effective arrangements to monitor adherence to the Mental Capacity Act” at the time of the visit and the trust was not carrying out regular audits to ensure that the Mental Health Act was being applied correctly. The report found that although the wards were “usually staffed to safe levels”, there was “high use” of temporary staff to cover vacancies, staff sickness and enhanced clinical need on the wards. It also shared that the systems for induction and training of temporary staff “did not always ensure that staff were familiar with the wards and the needs of the patients they were caring for”. While “most” patients told inspectors that the food was “good”, some said that “good quality food which met their cultural needs was not always available” and that they did not have access to spiritual support on the ward when they “would have liked this”. The CQC has instructed the trust to provide an action plan and to make improvements in response to the concerns found.
Bury North MP James Frith deemed the findings “unacceptable” and has written to the trust’s chief executive demanding “urgent answers and action” along with an immediate meeting. The Labour MP said: “The CQC’s findings are deeply troubling. “Older people in Bury deserve far better than wards that fall short on safety, staffing, and care. Source: Bury Times, 7th June 2025
Patients are dying and facing ‘horrible tragedies’ due to Manchester’s mental health care crisis, staff say
NHS workers in Manchester’s mental health services have accepted a deal for more funding and called off strikes – but they fear problems persist more widely in mental health teams across the country. Mental health services in Manchester have faced “crisis after crisis” and preventable patient deaths due to underfunding and “lack of compassion”, NHS workers have said. A group of employees at Greater Manchester Mental Health Trust have spent months striking to demand more support, funding and staff to continue their life-saving work. Backed by unions Unite and Unison, they have now accepted a deal of £750,000, followed by a recurrent £1 million in subsequent years, equivalent to 21 additional staff members. Claire Miller, a Unison representative who works in the Manchester early intervention psychosis (EIP) team said this is a “substantial investment”. “Without the right resources, we can’t help people recover,” Miller said. “This will make a real difference in the support we’ll be able to give families and how we’re able to respond.” However, there remain fears that the issues within mental health services persist in Manchester and across the country – particularly as the government recently reduced the proportion of NHS funding allocated to mental health services. Miller claimed community mental health services in Manchester are “still hugely under-resourced” and that the striking workers will continue to campaign for better funding more widely. “We need to support collective action and come together, because that’s how we win and resist. Not only have we resisted, but we’ve actually gained investment in this climate,” Miller added. “That needs to be coordinated on a national level.” Staff in Greater Manchester mental health services said they were concerned for patient safety.
Dr John Mulligan, a Unite union representative and clinical psychologist in the Manchester EIP team, believes problems persist. He claimed: “There’s been multiple horrible tragedies in our service and across the community mental health teams.” “The whole secondary care services are in an absolutely diabolical situation,” he said. Mulligan’s team works with 14- to 65-year-olds who develop the first episode of psychosis. EIP services have been found to reduce the risk of a person with psychosis attempting to take their own life from 15% to just 1%. However, Mulligan claimed there are “thousands” of people suffering with their mental health in Greater Manchester who are not getting the support they need. He said the caseload “just swells and swells” – staff are meant to have 12 patients allocated to them, but instead they have 25 to 30. “What happens then is all the sensitive, nice stuff that we’re supposed to be doing doesn’t happen. There’s been crisis after crisis,” Mulligan said. A Freedom of Information Request sent by striking workers to the trust and seen by the Big Issue revealed that 10 people had died while on a waiting list for mental health support as part of Greater Manchester’s ‘waiting well’ scheme since 2022, while 63 had been hospitalised. Mulligan said he is unable to share specifics of cases while investigations are ongoing but claimed the services are in “such a diabolic state that people are dying all over the place”. “It’s horrendous. There’s a massive waitlist of people who are severely unwell. They are just neglected and left at home,” he said.
Annabel Marsh, a former community psychiatric nurse who now runs a peer support group for people suffering with severe mental health conditions in Manchester, said that people used to be allocated a care coordinator who would regularly visit them – sometimes as much as weekly – but the service is “under-resourced” and it is no longer standard practice. When the group, Community Works, first started more than 10 years ago, each of the members had a care coordinator allocated to them, but now only three of the 35 members of the group receive this support. “Their situations haven’t changed. They still have ongoing issues with psychotic illnesses like schizophrenia, severe bipolar, with recurrent admissions, medication which has terrible side effects and causes quite a lot of physical issues as well, including type two diabetes and weight gain. These are issues which should be monitored. That just isn’t happening,” Marsh explained. “Some people have outpatient appointments with a psychiatrist, but that might be once or twice a year. If they go into crisis, there’s nowhere to ring for a rapid response. If people start to relapse, it’s extremely difficult to get a response quick enough to prevent hospital admissions. “Members of our group have had hospital admissions, almost all of which have necessitated the police getting involved because things have become so severe. People lose insight and awareness that they’re very unwell, because there’s no community services to step up support quickly.” In one recent case, a group member who had been “extremely at risk for a long time with symptoms of relapse” was receiving no support from mental health services. She was living in “deteriorated conditions” and was unable to look after herself.
Community Works provides a hot meal twice a week, because otherwise “people might not be eating at all”. Marsh, who is in her 70s, said one of the reasons she came off the nursing register is because she does not want to be “held responsible for what’s happening to people”. She said: “I do my best to alert services when things are going badly, but as an ex-nurse and now as a friend to the people who come to the group, it is deeply concerning when things go wrong, and it’s just constant.” Mulligan said he has heard “horror stories” from mental health teams across the country. Around 120 people die in England every day from preventable mental health conditions, according to the Royal College of Psychiatrists. “There’s a misconception sometimes about striking workers, that they’re disgruntled and at odds,” Mulligan said. “But actually, we’ve got an enthusiastic and skilful team, and we’re unionised. We give a shit. We’ve managed to have a coherent group for a few years, and we can see all of the damage and destruction, heartache and death that’s occurring locally, and we just have had enough. “Our team is fantastic, and although we’re brushed off the feet and struggling and facing lots of stress related to that, we are also motivated to fight to make things better. Most other teams don’t have that, and when we don’t, then what we are is complicit in a system that’s actually contributed towards death.
”Mulligan claimed that “many EIP patients” are gaining weight at a rate of up to 17kg in one year. “That’s 15 to 20 years of reduced life expectancy,” he added. “We’re the starting point for early intervention – but sadly, we’re complicit in and we’re contributing towards problems that continue in terms of physical health.” Unison North West regional organiser Paddy Cleary said: “Early-intervention mental health services are a lifeline for many at-risk people. Getting the right support at the right time can prevent a crisis, providing help long before someone reaches breaking point. This critical work goes on day in, day out.” He added that the “outcome of this dispute is fair and will help keep communities safe”. Research has found that if every patient with psychosis received effective early intervention, it would save the NHS £44m every year. A Department of Health and Social Care spokesperson said: “Too often, people experiencing mental health crises are not getting the support or care they deserve, and this government is taking action to change that.” They claimed to be transforming mental health services backed by an extra £680m in government funding – “hiring more staff, delivering more talking therapies, and getting waiting lists down”. It has also launched one of the world’s first 24/7 mental health crisis support services via NHS 111 and announced a £26m investment in new crisis centres.
Yet there are concerns this is not enough amid cuts to NHS services and as people wi th mental health conditions also risk losing their financial support while the government plans to tighten the eligibility criteria for disability benefits. Mulligan said: “If I had to say what the biggest problem is with the NHS mental health services, it would be a lack of compassion. We need staff to actually be able to do their job properly. We need staff to be skilled and comfortable, certainly. “But ultimately, what we need is compassionate decision making. We need time. We need resources. All of that costs a lot of money, but it’ll be very well spent, and it would be money that would save not just stress and human suffering, but lives.” He added: “Being in a system whereby we’re allowing or letting or we’re ignoring the fact that the most vulnerable in society are dying is intolerable, and it’s so unfair. So it is upsetting for all of our members. That’s one of the reasons that drove us forward to be out on strike.” Greater Manchester Mental Health Trust and NHS England did not respond to Big Issue’s requests for comment. Source: Big Issue, 4th June 2025
May 2025
Strike saves Manchester mental health service
Mental health strikers in Manchester have won their long running dispute over staffing and resources. The Unite and Unison union members—who are nurses, psychologists, social workers, support workers, welfare rights workers, CBT therapists and employment specialists—had been fighting local health bosses for more workers.They described the services provided by Manchester Early Intervention in Psychosis teams as “totally overwhelmed”. But after months of action bosses finally made a new offer of an extra £1 million in recurrent funding, which will pay for 21 staff across the service. Strikers this week voted to accept the offer and end the dispute. Unison branch secretary Claire Miller, said, “The support we have received, the friends we have made, the collective strength that’s pushed us through the winter and to this point where we have beaten the odds and shown that if we stand united, we can push those in power to make the right decisions.” She is right, and the victory has big implications for thousands of other NHS staff currently working in intolerable conditions. If a small team of determined strikers in Manchester can win on this scale, then the same must be true across Britain. Claire says that despite the victory, the wider fight for mental health services is far from over.“We pause today, to acknowledge some good news and the certainty that standing up together can work to effect the change we must demand,” she said in a statement. “Tomorrow, we must continue to fight for our six local community mental health teams. Please don’t wait until someone you love needs these services, only to then realise that they are not fit for purpose.” Source: Socialist Worker, 27th May 2025
Mental health NHS trust hit with urgent warning as whistleblowers spark safety fears: The inspection revealed breaches to people’s safety, and patients’ consent to care and treatment
A Greater Manchester mental health trust has been issued an urgent warning from the health and care watchdog after an inspection of its hospital wards. Pennine Care NHS Foundation Trust was visited by the Care Quality Commission (CQC) following safety concerns from whistleblowers and people using the units between June and October 2024. And according to the watchdog, these concerns about the wards for older people were proven to be ‘substantiated’ during the inspection in November last year. It revealed breaches to people’s safety and patients’ consent to care and treatment. The CQC also found that there were not enough staff with the right skills and training, according to its report published today (May 21).
The CQC has now issued the trust with a warning notice to make improvements to ‘ensure care was person centred, as well as providing enough staff with the right skills and training to meet people’s needs’ on the wards of concern. The trust has said it is ‘already delivering a robust improvement plan’ to ‘ensure lasting change’. Pennine Care provides inpatient, community and specialist mental health services across Bury, Rochdale, Oldham, Tameside, and Stockport, providing care to over 70,000 people as of 2023/24.
The trust operates inpatient mental health wards for a range of ages and diagnoses, including units at Fairfield Hospital, Stepping Hill Hospital, Tameside General Hospital, the Royal Oldham Hospital, and Birch Hill Hospital. Inspectors found that plans did not always show how care was focused on the patient, or that the views of carers or relatives had been taken into account on the wards for older people.
Some relatives and carers told inspectors that visiting times were restricted, and they were only allowed an hour with their relatives. ‘It was not clear that people who were not detained under the Mental Health Act could leave the wards freely’, the report also reads. ‘People did not always have a clear understanding of their rights’. ‘There was no quality assurance process to check whether compliance with the Mental Health Act was taking place for people’, the report added. However, the CQC said that levels of physical restraint and other restrictive practices such as seclusion were low. Alison Chilton, CQC deputy director of operations in the north west, said: “We found at our inspection of Pennine Care NHS Foundation Trust’s wards for older people with mental health problems, that some of the concerns we had received about the safety and quality of the service were substantiated. “We would like to thank people using the service, and staff for their bravery in sharing their concerns, as it helped us to have a better picture of the care being provided to people, which determines if we need to take any action to keep people safe, including carrying out an inspection. “On the wards we found there were times when there wasn’t enough permanent staff, and sometimes people were cared for by staff who weren’t familiar to them, particularly at night. Also, staff didn’t always have time to sit down and talk to people and give them the social interaction they need. “It was also concerning that staff weren’t always trained to provide care to people in a safe way. For example, many staff caring for people with dementia hadn’t received any dementia awareness training. “However, despite these issues, people and their relatives felt that wards were clean and well maintained which helped to keep them or their loved ones safe. “We shared our findings with the trust, so they know where improvements are needed, and since the inspection, they have informed us that they have started to make progress on these. We will continue to monitor the service closely, including through future inspections, to ensure people are safe.”
The CQC told the trust to submit a plan showing what action it is taking in response to these concerns. The watchdog says a plan has been put forward, and it ‘will continue to monitor the trust to ensure these improvements are made and people are safe while it happens’. Tim McDougall, executive director of quality, nursing and healthcare professionals at Pennine Care NHS, said: “We accept the findings of the CQC’s assessment of our older adult mental health wards and are fully committed to addressing the areas identified for improvement. Our focus is on delivering high-quality, person-centred care for all our patients. “While the inspection highlighted challenges, it also recognised positive practice – the compassionate care of staff, clean and safe ward environments, and our culture of safety and openness. “We are already delivering a robust improvement plan focused on strengthening clinical standards, patient engagement, staff training and ward leadership. We’re also improving compliance with mental health law, access to therapeutic activities and work to further embed a culture of kindness, respect and safety. “Importantly, we are working in partnership with patients, carers and staff to ensure lasting change. We’re proud our efforts are reflected in our latest NHS Staff Survey results which showed improvements across all seven themes, scores above the national average, and recognition as the best mental health and learning disability trust to work for in the north.” The overall rating for the trust’s wards for older people with mental health problems has dropped from ‘good’ to ‘requires improvement’. The service also dropped from good to requires improvement for specific elements, including how well-led, effective, caring and responsive it is. The safety of the service has been rated again as requires improvement. Pennine Care NHS Foundation Trust as a whole remains rated requires improvement overall. Source: Manchester Evening News, 21st May 2025
It used to be rare, now hundreds in mental health crisis wait days for beds in these A&Es
One nurse elsewhere in the country has told of how some patients become so distressed by delays that they have left to try and take their own lives. The number of Greater Manchester patients in mental health crisis waiting more than 12 hours for a bed have shot up by hundreds in the past five years. Three of the region’s biggest A&Es have seen people waiting more than 12 hours for a bed on a mental health unit to be found, after medics have decided to admit them, rise from a total of 115 in 2019 to 717 people in 2024. That’s an increase of just over 523 per cent.
One nurse elsewhere in the country has told of how some patients become so distressed by delays that they have left to try and take their own lives – followed out by nurses and firefighters attempting to stop them. But staff admit that A&E workers are so busy dealing with patients getting help with physical emergencies that mental health patients end up being looked after by security guards, instead of medical professionals. Freedom of Information requests to hospital trusts in England by the Royal College of Nursing (RCN) have revealed the appalling extent of these huge waits in some of Greater Manchester’s largest A&Es.
At Stepping Hill Hospital, the number of people languishing for more than 12 hours in A&E, waiting for a mental health bed to be found, rose from three people in 2019 to 117 in 2024. That’s an increase of 3,800 per cent. There were 20 such waits in the first two months of this year at the hospital’s A&E. At the Manchester Royal Infirmary A&E, nobody waited more than 12 hours for a bed after a medic’s decision to admit them to hospital in 2019 and 2020. Figures started creeping up to one person in 2021, 52 in 2022, and 340 in 2023. By the end of 2024, this figure had shot up to 463, with 90 such waits in the first two months of 2025. At the Royal Albert Edward Infirmary in Wigan, figures have risen from 112 people waiting more than 12 hours in 2019 to a height of 411 in 2022. This has since been brought down to 379 in 2023, and 252 last year. In January and February this year, 48 of the A&E’s patients waited longer than 12 hours for a bed. The RCN investigation includes testimonies from staff. Rachelle McCarthy, a senior charge nurse at one NHS trust, said: “It is not uncommon for patients with severe mental ill health to wait three days. Many become distressed and I totally understand why. I think if I was sat in an A&E department for three days waiting for a bed I would be distressed too.”
The director of nursing at a London trust said the “brightly lit, noisy” environment in her A&E was “close to torture” for those in mental distress and that patients often got so frustrated that they left, the RCN reports. In one London hospital a senior nurse described an incident where a mental health patient who’d been waiting for a mental health bed for three days became “incredibly aggressive, smashed a glass window, threatened staff and threw his own laptop across the room”. Once the situation was calmed down, he said: “I shouldn’t be treated like this.”“Everybody knows he is completely correct,” the nurse said.
The brother of one mental health patient who received treatment at an emergency department in the south east described his shock at finding out that his sibling had been monitored for 24 hours by a security guard rather than a health professional. “My brother needed care from a mental health professional, not to be guarded like he was a threat,” he said, according to the RCN’s report. A senior nurse in the south west of England said that a ‘whole team of senior nurses, security and firefighters’ as people leave during the painstaking waits and try to take their own lives: “Lots of people will just come and wait and be patient. But as you can imagine, some of them are in severe crisis. “They want to leave. They want to self-harm. They are massively distressed and struggling.” A spokesperson for NHS Greater Manchester, said: “NHS Greater Manchester recognises the significant impact of waiting over 12 hours for a hospital bed during a mental health crisis, not just on individuals, but also on their families who seek help at A&E. “We know that when it comes to mental health, it’s important that everyone has access to help when they need it the most. That’s why we are working closely with partners across the city-region, including hospitals, to invest in services that provide alternative options to hospital care, such as community-based crisis spaces. “These include drop in mental health hubs which don’t require an appointment or GP referral. We are also ensuring there is 24/7 mental health liaison in emergency departments. “While we have already made progress, we acknowledge there is still more to be done. Improving mental health services remains a top priority for us.” The RCN found at least 5,260 people a year in a mental health crisis have been facing the ‘degrading’ waits of more than 12 hours after a decision to admit – up from just over 1,000 in 2019. The number of people going to A&E for mental health emergencies has been growing overall, totalling 216,182 last year.
The recruitment of mental health nurses comes far short of demand, and the number of beds in mental health units has fallen by 3,699 since 2014, the RCN findings show. The NHS numbers obtained by the RCN gravely underestimate the waits longer than 12 hours and the number of people seeking help at A&E for a mental health emergency. Only 26 per cent and 52 cent of the 145 NHS trusts from which the union sought information provided figures on those two issues respectively. A Department of Health and Social Care spokesperson said: “People with mental health issues are not getting the support or care they deserve, and we know that many NHS staff feel burnt out and demoralised, having been overworked for years. “That’s why this government is investing an extra £680m in mental health services this year, to help recruit 8,500 more mental health workers, and put mental health support in every school. “We have also launched one of the world’s first 24/7 mental health crisis support services via NHS 111 and announced a £26m investment in new crisis centres, to ensure patients can get timely support from a trained mental health professional.” RCN General Secretary and Chief Executive Professor Nicola Ranger said: “Severely ill mental health patients waiting days for treatment in stressful and brightly lit A&Es is a scandal in plain sight. These conditions are not ‘the norm’ and nursing staff will not accept them. “If parity of esteem between mental and physical health is to mean anything, then these utterly degrading waits must end. “Nothing less than urgent and sustained investment in community mental health nursing can ensure everybody gets timely care in the right place. That is how you turn people’s lives around and ease pressure on emergency departments.” Source: Manchester Eve Ning News, 14th May 2025
April 2025
Family of man who committed murder after escaping from mental health unit say they were ‘failed’ by NHS trust
Joshua Carroll escaped from the Park House in Manchester on 21 occasions and after doing so in September 2022, he beat a man to death in a park. The Carroll family say they had repeatedly complained to the trust and asked for help. At the time of the attack, Joshua was in the care of Greater Manchester Mental Health Trust (GMMH). He was being treated as an inpatient at Park House, a unit which has now closed down. Joshua’s mum and sister say he escaped from the unit 21 times – and they repeatedly complained to the trust and asked for help. Leanne Carroll, Joshua’s sister, told Sky News: “The night it happened, Joshua had come to my house. And it was just a normal ‘oh Joshua has escaped from hospital again’. Nothing appeared any different.” She says they didn’t find out about what had happened until Joshua was arrested weeks later – and “everything fell apart from there”. “My heart broke,” said Joshua’s mum, Julie Carroll. “It’s just a horrible, horrible situation.” Joshua had been diagnosed with conditions including schizoaffective disorder, and had been in and out of inpatient care for around 15 years, his family said. They showed me more than 20 pages of complaints and responses from GMMH about his repeated escapes, dating back eight years before the murder. After Joshua’s fourth escape from Park House, his family asked for him to be moved to another unit, saying they were concerned about security. This didn’t happen, with the trust citing capacity issues. His family complained once again about his escapes just five weeks before the murder, in August 2022. “We are very, very angry and disappointed,” said Julie. “You think if your child is in hospital, and they are very poorly, that they are going to be looked after – they will be safe and they will be secure. But that wasn’t the case for Josh.” Although Joshua was convicted of murder, Leanne says his family hold GMMH partly responsible. “If you had done your job properly – none of this would have happened,” she said. “Two families wouldn’t have been destroyed and so many hearts wouldn’t have been broken.”
Since 2022, GMMH has been served with several Section 29A warning notices by the Care Quality Commission. These are issued when the commission decides a service needs to make significant improvements, and there is a risk of harm. In the case of GMMH, their concerns included “ward security systems not consistently keeping people safe”. Dr John Mulligan is a clinical psychologist for GMMH, working in the community for the early intervention in psychosis service, and a representative for the union Unite. “Thankfully, violent incidents among our service users are quite rare, they are much more likely to be the victims of violence and aggression,” he said. “But serious incidents are happening regularly. Far too regularly. “It’s very upsetting for staff and for patients and families.”
Salli Midgley, chief nurse at the Greater Manchester Mental Health NHS Foundation Trust said: “On behalf of GMMH, we express our heartfelt condolences to Headley Thomas’s loved ones at this very sad time. “Our thoughts and sympathies remain with everyone who has been affected by this most devastating incident. We are deeply sorry that it happened while Joshua Carroll was under our care. “Under the trust’s new leadership, we have been working closely with NHS England, our commissioners and the CQC to create better, safer and well-led services for all.” She continued: “A huge amount of progress has already been made but we know we still have a lot to do to improve our services.”As part of this work, we are currently carrying out an in-depth investigation into the care and treatment provided to Mr Carroll, and the circumstances leading to Mr Thomas’ death, the findings of which will be shared with NHS England. “We are unable to comment further on this case whilst the investigation is ongoing.” Barry Thomas’s family told Sky News mental health is a very serious issue – but they believe Joshua Carroll tried to “play down his actions”. They said: “Let’s all remember that a life was taken. Our brother, father, and uncle. The evidence the police gathered was in plain sight for all to see. “We, the family, would like to thank all the police involved for the work they have done, in bringing justice for Barry.” Source: Sky News, 17th September 2025
Charlotte Parry’s death contributed to by neglect on part of Greater Manchester Mental Health trust, inquest jury finds
The jury’s findings brought an end to an emotional two-week inquest at Manchester Coroner’s Court (pictured). Credit: Alex Blair / Garden Court North Chambers. The jury’s findings brought an end to an emotional two-week inquest at Manchester Coroner’s Court (pictured). Credit: Alex Blair / Garden Court North Chambers. Earlier today (11 April), an inquest jury found that neglect on the part of Greater Manchester Mental Health (GMMH) NHS Foundation contributed to the tragic death of Charlotte Parry on 6 February, 2022. Charlotte was detained under the Mental Health Act 1983 on the Bronte Ward of Wythenshawe Hospital due to her high risk to self and diagnoses of Emotionally Unstable Personality Disorder, Obsessive Compulsive Disorder and Generalised Anxiety Disorder. The jury made numerous critical findings in relation to the care provided to Charlotte during her time under GMMH care, including in relation to her observation levels, the return of items used to ligature, delays in applications for funding for specialist treatment and ward systems for managing ligature risk, finding that these caused or contributed to Charlotte’s death. The jury also made a number of critical findings in relation to the Trust as a whole, including that the systems in the Trust for managing ligature risk were not adequate, and that this possibly caused or contributed to Charlotte’s death. They further found that there were significant and systematic failures in the Trust and incompetence at a senior leadership level. The jury’s conclusion brought an end to an emotional two-week inquest at Manchester Coroner’s Court. Carol Parry, Charlotte’s mother, said in a statement: “We as a family are absolutely devastated. For the jury to conclude neglect by GMMH contributed to Charlotte’s tragic death makes this even more unbearable. To date, we have not received any sort of apology for their significant and systematic failures including numerous critical findings in relation to Charlotte’s care. We would like to thank HM Coroner Mr Appleton, the jury and our legal team (Kelly Darlington of Farleys Solicitors and Lily Lewis of Garden Court North Chambers) for their professionalism and kindness. We are pleased that Professor Shanley and the CQC [Care Quality Commission] are closely monitoring GMMH’s practices and hope that changes continue to be made to protect other patients within their care. We as a family are not making any further comment at this time as we continue to navigate life without our beautiful Charlotte.” Throughout the inquest, Garden Court North’s Lily Lewis rigorously questioned dozens of Trust witnesses called to give evidence on the circumstances surrounding Charlotte’s death. Lily and Kelly Darlington of Farleys Solicitors represented Charlotte’s family. Source: Garden Court North Chambers, 11th April 2025
An inquest finds Greater Manchester Mental Health’s lack of care contributed to a suicide
(EXTRACT) … In its conclusion, the jury said that the lack of risk assessment related to the bag, and the chest of drawers not being identified as a ligature risk, contributed to Charlotte’s death. Other factors, like it taking three minutes for ward nurses to call Dr Grice, were found not to have contributed to Charlotte’s death but were still deemed significant.
Appleton, the coroner, left the option open for the finding of neglect. The threshold to do so is quite high. It means the evidence suggested there had been a gross failure to provide basic care. “For a jury to find that is a very stark and powerful finding,” Lewis, the lawyer, told me afterwards. And in Charlotte’s case, they did find that neglect contributed to her death.
In a statement to The Mill, the Parry family said: “We as a family are absolutely devastated. For the jury to conclude neglect by GMMH contributed to Charlotte’s tragic death makes this even more unbearable. To date, we have not received any sort of apology for their significant and systematic failures including numerous critical findings in relation to Charlotte’s care.”
When we approached GMMH for comment, asking for their response to the family’s statement and whether they would apologise, Mike Hunter, Interim Chief Medical Officer said:
“On behalf of GMMH, I would like to say how truly sorry we are for the failings in the care and treatment we provided for Charlotte Parry. The death of a loved one is always a tragedy, but to learn that neglect contributed must have been devastating for Charlotte’s family and loved ones, and we will be contacting them personally to reiterate our apology.
“Since Charlotte’s death in February 2022, under the Trust’s new leadership, we have been working closely with NHS England, our commissioners and our regulators to create better, safer and well-led services. Our Trust-wide recovery plans address all nine recommendations for GMMH from Professor Shanley’s independent review published in 2023.”
“We would like (to) say again how very sorry we are that we did not do more for Charlotte and her family.”
Source: The Mill. 17th April 2025
‘Innovative’ scheme helps people with mental health needs home in Greater Manchester
People with severe mental health needs are being rehabilitated into the community in an “innovative” scheme to reduce the number of people spending extended periods in hospital.The project, in Greater Manchester, aims to speed up discharge for patients on mental health units and get th em home safely. Many of them have been in hospital for years.The Pennine Care Community Rehabilitation Team says its success has also led to a significant reduction of its out-of-area placements so patients can receive care closer to home.
Muhammad Khan was 23 when he was diagnosed with paranoid schizophrenia.Now aged 41, he has been sectioned multiple times, spending a total of 10 years in hospital. His latest and longest hospital stay was for six years. Muhammad said: “Prior to becoming unwell, I had a lot of plans, I had a lot of ambitions. I wanted to become a writer. I wanted to start a family. I wanted to work. I wanted to study. “But because of going in and out of hospitals – they call us revolving door patients – because of that I wasn’t able to complete my education or fulfil a lot of my ambitions. ” “I was institutionalised because I was in the hospital system for six years.”But things did improve for Muhammad after he began working with the Pennine Care Community Rehabilitation Team.They offer ongoing support to people with long term mental health needs when they leave hospital. The aim is to help them integrate safely back into the community and prevent relapses.
David Hill is Muhammad’s peer support worker and part of the Community Rehab Team which worked with him for the past 18-months. He said: “Often people are worried and scared about coming back into the community. “They want to do it but they are worried about how they’ll cope. “Some people we are working with have been in hospital for 20, 25 years.” “I think the big challenge is the change in life experiences from an environment where there are lots of restrictions and lots of things are done for you, to an environment where you have a lot more freedom in your life but if it is not managed correctly that can be a point when people really struggle and there is a risk of relapse taking place.” Muhammad’s been living in supported accommodation for the past year. He believes the intensive level of support he has received from the team has been key to him staying well and staying out of hospital. Source: ITV X, 17th April 2025
March 2025
February 2025
Healthcare workers in Manchester strike over ‘deadly’ mental health crisis
Nearly 20 healthcare professionals went on strike yesterday to call for improved mental health services – insisting people are dying due to budget cuts in Manchester. The demonstrators, from the Unison and Unite unions, gathered in the city centre with placards, banners and flags to protest against the Greater Manchester Integrated Care Board (ICB). The group, who work for Manchester Early Intervention in Psychosis service (EIPs), blamed budget cuts and excessive expenditure on private contracts for contributing towards deaths in the city at a “disproportionate rate”. Protesters described the general state of the NHS as “deplorable”. The group, who demonstrated outside the Greater Manchester Combined Authority offices on Oxford Road, described the region’s mental health services as among the most deprived and underfunded in the country. A Unite rep claimed: “Manchester suffers twice as many deaths from mental health illnesses than the rest of the country.” More than 40,000 deaths in England per year can be attributed to preventable mental health illnesses, say protesters. And NHS reports from 2022, the most recent data available, suggested the number of those experiencing a mental illness in Greater Manchester was disproportionately higher than the general population. Post-pandemic government data indicates a continuing rise. Dr John Mulligan, Unite rep and clinical psychologist at Manchester’s EIPs, said: “People are genuinely dying in Manchester as a direct result of the lack of investment in preventive medicine.” The ICB, which is funded by the GMCA, has been contacted for comment. Source: Mancunian, 27 February 2025
January 2025
People with severe mental illness twice as likely to die early in Manchester than anywhere else
It comes as Greater Manchester is facing a crisis within its mental health services.People with severe mental illness are more likely to die prematurely in Manchester than anywhere else in the country. For every 100,000 people with severe mental illness, there were 233 deaths in Manchester. That means people with longstanding mental health conditions were more than twice as likely to die prematurely than the national average.More than 130,000 adults with a severe mental illness (SMI) – the term for debilitating psychological problems that often leave sufferers struggling to carry out daily tasks or work – died prematurely in England between 2021 and 2023.
That’s around 18,000 more deaths than in the three-year period from 2017 to 2019, just before the Covid-19 pandemic and the lockdowns that followed, leaving many people isolated and cut off from essential support. During that time, the rate of premature deaths in England increased from 98 deaths for every 100,000 people with SMI in 2017-19 to 111 deaths.
The NHS in Greater Manchester said: “We will look closely at the latest set of data release to better understand if there was anything that could have been done differently which we will then feed into our current programmes of work.” Outcomes for people with severe mental illness are far worse in some parts of the country than others. From 2021 to 2023, more people with an SMI died prematurely in Kent than in any other county council area in England, a total of 3,700. But when compared to the size of the severe mental illness population in each area, premature deaths are far more likely in Manchester, at 232 for every 100,000 people with severe mental illness. Next was Blackpool (232 deaths per 100,000), and then Middlesbrough (213), Stoke-on-Trent (199), Kingston upon Hull (198), and Liverpool (196). With the exception of Stoke-on-Trent (West Midlands), all the areas with the highest premature death rates of people with SMI are in the north west or north east, and all have high levels of deprivation.
Salford, Bury and Rochdale rank seventh, eighth, and ninth respectively in the top 10 areas of the country where the rate of deaths is highest – meaning Greater Manchester boroughs make up four out of the top 10 of these locations of highest rates of deaths. In contrast, the areas with the lowest rates of premature death are all more affluent areas in the South. Oxfordshire had the lowest rate, with 55 deaths per 100,000 people, four times lower than in Manchester. The deaths are mainly from serious illnesses, including cancers and heart, liver, and respiratory diseases – not directly as a result of serious mental illness. However, poor physical health is more common among people with severe mental illness, and it is estimated they die on average 15 to 20 years earlier than the general population. Smoking rates are high among people with severe mental illness, and people struggling with long-standing mental health problems may also find it harder to keep on top of a treatment plan. They are also at increased risk of suicide. Source: Manchester Evening News, 23rd January 2025
‘Concerns remain’ at trust where patients abused
A mental health trust where a “toxic culture” saw patients abused in 2022 has been rated as inadequate again despite some improvements.
The secure unit the Edenfield Centre in Prestwich, Greater Manchester, was the subject of a BBC Panorama investigation which revealed how patients were humiliated and bullied. In its latest report into forensic inpatient and secure wards at the Greater Manchester Mental Health NHS Foundation Trust (GMMH), the Care Quality Commission (CQC) found issues with patient safety and pressures on staff and said some still felt unable to speak up about their concerns. GMMH, which runs Edenfield, said it accepted the findings and had “worked at pace” to address the problems identified. Inspectors from the CQC made an unannounced inspection in April and May 2024, giving the trust an overall rating of inadequate. Alison Chilton, its deputy director of operations in the north, said: “The trust’s processes didn’t always ensure the environment was safe for people. “We found some wards which carried out 15-minute security checks to keep people safe had gaps and missing signatures in their records.” ‘Cultural divide’ Other issues included staff being asked to carry out observations for hours without a break, ligature risks not being identified and unsafe management of medicines. Ms Chilton said there was also evidence of restrictive practices across the wards within the trust, which also includes centres other than Prestwich. “The service had imposed blanket restrictions without evidence to demonstrate the decision-making behind this, or that these were being kept under close review,” she said. Management had expressed concerns about managing an influx of new staff, while inspectors were told of a “cultural divide” on some wards with complaints of bullying. However there was signs of “cultural improvements” in regard to learning, safety and leadership and inspectors saw staff treating patients with compassion. GMMH said it was “disappointed” that the CCQ report had taken so long to be published but accepted it was an accurate depiction of the situation at the time. Salli Midgley, chief nurse at the trust, said: “We will always be sorry for the failings in the past but under the Trust’s new leadership we are focussed on getting the fundamentals of care right every time for our service users, their families and carers.” Some staff at the Edenfield Centre were sacked after the Panorama investigation was broadcast. The programme sparked an independent report, led by Prof Oliver Shanley OBE, who found the trust repeatedly missed opportunities to act on concerns and had a culture of “suppressing bad news”. It said Panorama had exposed the “most shocking abuse and poor care” of vulnerable patients and that concerns raised by families were “not always taken seriously”. Source: BBC News, Manchester, 18 January 2025
December 2024
A GMMH Trust mental health nurse who sexually assaulted a patient on a ward has been jailed
Matthew Wharton was arrested in May after the woman reported that he had “repeatedly raped” her at Laureate House, a mental health facility next to Wythenshawe hospital in Manchester, police said. The 37-year-old agency nurse pleaded guilty to a range of sexual offences against the woman. Wharton was jailed for four-and-a-half-years at Manchester Crown Court and was also given a 10-year restraining order. Source: BBC News, 17th December 2024
GMMH Mental health patients ‘abandoned’ on waiting lists
Staff at Greater Manchester Mental Health Trust said people with severe long term illnesses being looked after in the community were not getting the help they needed Hundreds of patients feel they have been “abandoned” because the resources are not there to care for them properly, it has been claimed. It comes as a group of employees at Greater Manchester Mental Health Trust are again striking this week to protest what they say is a lack of funding and support. They say some people with severe long term illnesses being looked after in the community are stuck on long waiting lists and not getting the help they need. NHS Greater Manchester said it knew it was an area which required urgent attention and it was committed to solving the problem. Source: BBC News, 11th December 2024
Back vital Manchester mental health strike
Mental health strikers and supporters on the picket line in Manchester this week Around 40 workers for Greater Manchester Mental Health services are striking this week over understaffing and underfunding. The Unison and Unite union members work for the Early Intervention in Psychosis teams. Claire, a Unison rep and striking mental health social worker, explained what is at stake. “There is a massive shortfall in staffing. And we don’t have the staff we need to be able to deliver safe and effective care for people,” she told Socialist Worker. “We’ve been fighting for it for four years. Each time we’ve thought we had an agreement for more investment, it’s not gone ahead. So we have made the decision to strike to make this happen. “There’s not enough staff to be able to do the things that really make a difference in terms of people’s recovery. “Instead, we end up relying on medication too heavily, which comes with its own health risks and side effects. “That means unnecessary hospital admissions, often in private hospitals, which cost thousands of pounds a night. That’s money straight into the hands of private providers.” Another striker explained, “It’s a big secret that mental health services are struggling, that they are underfunded and understaffed. You wouldn’t know that, unless you are a staff member or a service user.” There was solidarity from the local community. One supporter said, “Having used mental health services for years, I’ve come here to show support for the strikers. I know that our services are not able to properly provide preventative care.” Source: Socialist Worker, 10th December 2024
Murder suspect absconded eight times, inquest told
A woman who stabbed a pensioner to death after absconding from a mental health unit was not thought to pose a threat of violence to others, an inquest has heard. Emma Borowy, 32, killed 74-year-old Roger Leadbeater as he walked his dog, Max, in a park in Sheffield on 9 August 2023.
Sheffield Coroner’s Court heard Ms Borowy, had absconded from a ward at Royal Bolton Hospital on numerous occasions before she attacked Mr Leadbeater, and was twice found with knives when she was located by police. However, Dr Hayley Thomas, a consultant psychiatrist, said concerns associated with her going missing were connected to her “vulnerability, risks to her health, and substance misuse” and the fear she was at risk of committing violence in the community “wasn’t a real concern for us”. The inquest heard how Ms Borowy, who had been diagnosed with schizophrenia and psychosis, was sectioned in October 2022 and admitted to Oak Ward at the Royal Bolton after she was arrested for killing two goats with a knife. Dr Thomas said Ms Borowy, who had been known to mental health services since 2008, had told police she had killed the goats “as a way of ensuring her own survival”. Ms Borowy admitted the offence, but showed no remorse, the hearing was told. Police officers later found teddy bears floating in a bathtub when they searched her house, as well as a “shrine” to unicorns. She had previously told social workers she could communicate with animals, with Dr Thomas telling the hearing they had been concerned Ms Borowy had been sleeping in a forest prior to her hospital admission. The hearing was told that Ms Borowy went on to abscond from secure units at the Royal Bolton on at least eight occasions.
After going missing from the ward on one occasion she was found by police on the A57 in the Rother Valley, the inquest heard.
According to officers present, she was in possession of a Stanley knife and said she had “thoughts to kill others and mentioned a bloodbath”.
Dr Thomas said the Greater Manchester Mental Health NHS Foundation Trust had been “unable to take it further” after Ms Borowy denied making the comment. Dr Thomas said that after leaving the unit another time, Ms Borowy told hospital staff she would “kill someone” if she returned to the ward. Dr Thomas said that during a conversation they had two months prior to Mr Leadbeater’s death, Ms Borowy “wasn’t accepting of her diagnosis” and she had also been reluctant to take medication for her psychosis. The inquest was told that despite her repeated attempts to escape, Ms Borowy continued to be allowed periods of leave from hospital on a regular basis. Dr Thomas said this was extended in a bid to reduce the frequency of her absconding. “Patients don’t like to be detained against their will in hospital,” she said. The decisions hospital staff made to continue discharging Ms Borowy “were very clearly thought through in relation to trying to manage somebody that would most likely be going back into the community,” Dr Thomas said. “You can’t punish patients for going AWOL. It’s a constant balance between the fact that you are detaining patients against their will and working with them therapeutically to move forward to move out of hospital. “We were struggling with a lady who didn’t want to conform to any of the work we were trying to do.” Ms Borowy was charged with murder, but died in prison before she stood trial.
The inquest continues. Source: BBC News, 9th December 2024
Inside Greater Manchester’s failing mental health trust
GMMH, Greater Manchester’s troubled mental health provider remains ‘inadequate’ following the latest inspections of its services. Inspectors at the Care Quality Commission (CQC) found several wards run by the Greater Manchester Mental Health (GMMH) Trust were unclean and poorly maintained, with some patients feeling ‘unsafe’. Blood was found on the bathroom wall of one ward in Salford where toilets and sinks were described as ‘dirty’ while windows were boarded up and walls left unpainted at a unit in Urmston. Gaps were found in medication records with one patient found to be taking an incorrect dose. Some patients also told inspectors about ‘assaults’ taking place on the wards, with staff not always intervening in conflicts or when others patients act aggressively. Source: Manchester Evening News, 4th December 2024
Major reforms to mental health services announced amid GMMH trust’s failings
Manchester council has announced major reforms to mental health services amid another damning report into an NHS trust. The Greater Manchester Mental Health (GMMH) trust remains ‘inadequate’, two years after claims of patients being abused by staff at a unit were exposed. Manchester council has now decided to change the way it works with the trust in the hope of improving services. Adult social care mental health workers in the city’s neighbourhood teams who are currently deployed to GMMH will now answer to the town hall directly. The change, which is expected to take effect next year, will affect all community mental health teams in the city. It comes after the Care Quality Commission (CQC) published the findings from its latest inspections of the trust today (December 4). Inspectors visited 23 acute wards for adults and psychiatric intensive care units in March, ruling those services are ‘inadequate’. The 10 long stay or rehabilitation mental health wards for adults were inspected later in the year ‘require improvement’, inspectors said. They found several wards were unclean and poorly maintained, with some patients feeling ‘unsafe’. Some patients told inspectors about ‘assaults’ taking place on the wards, with staff not always intervening in conflicts or when others patients act aggressively. Gaps were found in medication records with one patient found to be taking an incorrect dose. Inspectors also raised concerns about staffing levels, training and fire safety and found that half of the health and safety inspections were at least three years out of date. Source: Manchester Evening News, 4th December, 2024
GMMH Trust ‘inadequate’ after patients smoke on wards
Mental health wards where staff were unable to stop patients smoking and did not know what to do when fire alarms went off have been ordered to “rapidly improve”. Inspectors found a paper towel stuffed into a smoke detector during visits in March to acute wards for adults and psychiatric intensive care units in Greater Manchester. The service, run by Greater Manchester Mental Health NHS Foundation Trust, has been downgraded to inadequate by the Care Quality Commission (CQC). Salli Midgley, the trust’s chief nurse, said staff were “working hard” to make improvements after the failings highlighted by the watchdog. Alison Chilton from the CQC said inspectors found fire safety was a particular issue on the wards, as staff lacked fire safety training and regular drills did not take place. They found oxygen cylinders loosely attached to walls in some areas, with fire risks “not managed well” in wards that were “not always clean or well maintained”. When a fire alarm was set off during their visit on one of the wards, the response was “uncoordinated and confused”, the watchdog’s report said. Source: BBC News, 4th December 2024
November 2024
Striking against mental-health cuts in Manchester
Mental-health provision in Manchester needs substantial more funding to function safely, yet authorities are trying to cut more from the service, reports Counterfire. Early Intervention in Psychosis workers from Greater Manchester Mental Health (GMMH) have started another two days of strike action Friday (8 November) and then again on Monday (11 November). This is a principled dispute over unsafe staffing levels and underfunding. Unison and Unite strikers at the picket Friday talked about GMMH’s allowing dangerously low staffing levels in the Early Intervention teams. This puts severe stress on workers and means the needs of seriously unwell service users cannot be adequately met. This is of huge concern but especially so due to rising mental-health deaths across the country. They also talked about the wider issues in GMMH Community Mental Health provision, such as: Freezes on vacant posts and over-reliance on temporary agency and bank staff, with no consistency of care. The same regulators and commissioners demanding service improvements, refuse to pay for the skilled staffing these services need.
Plans for millions of pounds worth of budget cuts across GMMH services
Up to £30 million a year in out-of-area hospital beds goes straight into the pockets of private health companies. This is due to a lack of community provision and massive cuts to GM NHS mental-health inpatient beds since 2020.
Greater Manchester Mental Health are aware of the major issues in Early Intervention services and promised additional ‘ring-fenced’ funds. Unfortunately, they have failed to provide this. Additionally, since industrial action started (there was a previous one-day strike on 16 October), they have not met with strikers and their union representatives.
Union representatives have met with the Mayor of Greater Manchester, Andy Burnham, on Thursday 7 November, who said he will look into the issue. The workers plan further strike action until their demands are met. Demands include:
- there being substantial investment in Manchester EIS, so funding is in line with the NHS England workforce calculator. This is what the actual evidence base says is needed (and at last count was £1.03 million). This is the same amount of national money that had been ring-fenced for Manchester EIS but was never received.
- a big investment in Manchester’s Community Mental Health Teams. GMMH and the Integrated Care Board (ICB) that oversees the funding for GMMH (and Greater Manchester) are currently in special measures. They have been told by NHS England to repay millions in so-called ‘debt’.
- Strikers want Andy Burnham, politicians and anyone else in a position of power, to help resolve the funding issues and ensure these essential NHS mental-health services get the investment they urgently need
So it’s important that as many people as possible support the strike actions. Strikers are currently looking at ways supporters can help them put further pressure on GMMH and the funding body. The workers were back out on strike on Monday 11 November. See the Unison Greater Manchester Mental Health Facebook page to stay up to date with progress. Source: Counterfire, 12th November 2024
Patients left feeling abandoned by ‘broken’ Greater Manchester mental health care system
Patients and staff at a Greater Manchester mental health service have told ITV Granada the service is broken, with those who need support feeling ‘abandoned’. It can be revealed that there are currently more than 500 people with severe mental health issues waiting on a list and not receiving the help they need. And even when they are seen, patients say they’re only offered short-term fixes, with no ongoing support. Dr John Mulligan, a Unite representative and Psychologist who works in the Early Intervention Service, says he believes the system is broken. “If your family member becomes unwell, you’re very unfortunate living in Manchester”, he said. “The ratio of staff to service users is appalling in Manchester, so much so that it’s an abusive system we’re in at the moment where people are not getting what they need but there is a bit of a pattern or a repetitive cycle where some of our service users can’t even talk about positives in their week, they can’t even talk about recovery and things that are going well because they’re afraid of being discharged.” Source: ITVX News, 18th November 2024
Greater Manchester mental health workers to continue their walk out over ‘dangerous staffing levels’ and ‘underfunding’
Early-intervention workers will stage two strikes over what they say is their employer’s failure to improve staffing levels. A picket line will be in place tomorrow outside the GMMH Trust HQ at Prestwich Hospital. Mental health staff in Manchester are to to walkout in a dispute over unsafe staffing levels and ‘underfunding’. Two 24-hour strikes are planned on Friday (November 8) and Monday (November 11). The early-intervention workers, employed by Greater Manchester Mental Health NHS Foundation Trust (GMMH), are represented by UNISON and Unite. The two unions are taking action over what they say is their employer’s failure to improve ‘dangerous’ staffing levels despite the trust’s previous commitment to seek new funding to address the issue and ‘strenuous workloads.’According to UNSION and Unite, staff shortages are not only placing extra pressure on the workforce, but are also harming patient care. This is the second round of strikes, following a one-day walkout last month. Source: Manchester Evening News, 7th November 2024
October 2024
GMMH mental health staff stage strike protesting against underfunding and staffing levels
GMMH mental health workers say they have been forced to take strike action because poor staffing levels and a lack of funding is putting live at risk. Union members in the Early Intervention in Psychosis teams across Greater Manchester walked out for 24 hours on Wednesday, 16 October. With a 60% above average need for mental health services in Manchester, staff say a lack of investment is “unsafe”. Professor Anandi Ramamurthy, co-founder of CHARM – a group for better holistic mental health services, says she feels her daughter, who was diagnosed with psychosis, was failed by the service when she was in need. “I am delighted that early intervention workers are striking”, she said. “I think it’s really important for people to remember that this is not about pay.”They’re not asking for things for themselves. They’re saying that this service is unsafe and it’s absolutely imperative that this situation changes before the crisis gets any worse.” The early-intervention workers, employed by Greater Manchester Mental Health NHS Foundation Trust (GMMH), are represented by UNISON and Unite. Source: ITV News, 17 October 2024
Mental health care service on its knees – doctor
Dr John Mulligan says there has been a “serious decline” in support for people needing mental health care which is “unacceptable” A city’s community mental health service is “on its knees” and patients are dying due to the lack of staff and funding, according to a clinical psychologist. Dr John Mulligan, who works for one of Manchester’s Early Intervention in Psychosis teams, said union members were set to strike next week over concerns for patient safety due to understaffing. It comes as a freedom of information (FOI) request by the BBC revealed the North West’s NHS hospital trusts spent £45m more on private mental health care beds in the last three years. Source: BBC News, 10 October 2024
Andy Burnham pleads with mental health workers ‘not to follow through with industrial action’
The mayor said he would meet with mental health workers to address the issue. Mental health workers are gearing up to go on strike next week over care standards and understaffing. Mental health workers are gearing up to go on strike next week over care standards and understaffing. As mental health workers prepare to go on strike over ‘dangerous’ conditions for patients, Andy Burnham has pleaded with them ‘not to follow through with industrial action’. The Greater Manchester mayor offered to work with mental health teams to ‘discuss issues’. Union members in Manchester’s Early Intervention in Psychosis teams are reportedly set to strike on 16 October, due to staffing levels at ‘lower than acceptable standards’, leaving patients at risk. Source: Manchester Evening News, 10 October 2024
Construction of £105m GMMH mental health hospital completes
North View, a 150-bedroom in-patient mental health unit, will open its doors next month after works were finalised this week.The purpose-built project has been constructed by contractor IHP, a joint venture between VINCI Building and Sir Robert McAlpine. The project’s designer, Gilling Dod Architects, hailed the development as “the single biggest investment in mental health services in Greater Manchester for a generation” in a press release. On Friday, the £105m building was formally handed over to the Greater Manchester Mental Health NHS Foundation Trust, which will operate the site. The hospital will provide nine single-sex wards, six wards for adults of working age, a psychiatric intensive care unit, a rehabilitation ward, and an older adult ward. North View will replace Park House, an inpatient ward at North Manchester General Hospital in Crumpsall. Source: Place North West, 9 October 2024
Homeless in Greater Manchester face mental health epidemic
More than three-quarters of homeless people have mental health problems according to new data released by a Salford anti-poverty charity. Caritas collected data between February and March 2024 which revealed a stark disparity in health and well-being across Manchester, Bury and Salford between those who are homeless, or at risk of becoming so, and the general public. A staggering 73% self-identified as having at least one physical health condition, compared with 50% of the general population, begging the question: why aren’t we doing more to protect the vulnerable in our society? Amanda Croome, head of homelessness for Caritas Salford, said: “The huge difference in these figures shows a real issue that needs addressing before it’s too late for many. “It’s completely unacceptable.”But the grim reality of a life in poverty doesn’t end there – 69% of homeless, or at-risk-of-homelessness, interviewees said they had a mental health diagnosis. Yet only 19.2% said they had a mental health worker. And a concerning 34% admitted they had felt suicidal or had self-harmed in the last twelve months. Source: Mancunian Matters, 4 October 2024
September 2024
The region’s mental health services have sent people so mentally unwell they need full time care in hospitals more than 200 miles away from home
‘We’ve been sending seriously mentally ill people more than 200 MILES away to Taunton because there are no hospital beds in Greater Manchester’
‘If it was, to me, a complete scandal that we were sending people as far as Taunton… It’s a long way, not just for patients but for their families’, says the top boss of Greater Manchester’s NHS
Greater Manchester’s NHS has been sending seriously mentally ill people as far as Taunton, in Somerset, to get treatment because of a shortage of hospital beds and staff in Greater Manchester.
The region’s mental health services have sent people so mentally unwell they need full time care in hospitals more than 200 miles away from home, which the region’s top NHS boss has slammed as a ‘scandal’. Controversy around ‘out-of-area mental health placements’ has been swirling for more than a year in Greater Manchester, with the most senior doctors raising concerns about the safety of patients being treated so far from their families and familiar surroundings.
The costly far-flung beds were also cited as a main reason for the financial crisis Greater Manchester’s NHS has been mired in over the last year. There are still 81 people currently being treated as mental health inpatients in hospitals outside of Greater Manchester, according to latest figures. Source: Manchester Evening News, 10th September 2024
More mental health detentions in Greater Manchester last year
Last year saw a rise in detentions made under the Mental Health Act in Greater Manchester. Under the act, people with a mental disorder may be formally detained in hospital, or “sectioned”, in the interests of their own health or safety, or for the protection of other people. Mental health charity Mind said legislation around mental health must be brought into the 21st century to address the “overuse of restrictive, forceful practices”. Recent NHS figures show an estimated 3,435 detentions were made in the year to March within the NHS Greater Manchester Integrated Care Board area – up from 3,325 the year before. Across England, 52,460 new detentions were recorded last year, up from 51,310 in 2022-23. Nationally, black people continued to face a higher rate of detentions under the act – over three times the rate of white people. In Greater Manchester black people had a detention rate of 212.5 per 100,000 people – two times the rate of 103.8 per 100,000 for white people. Source: Wigan Today, 21 September 2024
Two years after shocking ‘patient abuse’ the troubled hospital unit at the centre of a scandal is set to reopen
The Edenfield Centre on the grounds of the former Prestwich Hospital came to national attention after claims that the vulnerable patients there were being abused by staff Claims were made in a Panorama programme that patients at the Edenfield Centre were abused The troubled epicentre of a mental health care scandal is expected to reopen after shocking abuse revelations saw it shut for two years, bosses have said. The Edenfield Centre on the grounds of the former Prestwich Hospital came to national attention after claims that the vulnerable patients there were being abused by staff. In a BBC Panorama programme which aired at the end of September 2022, staff were filmed slapping and pinching mental health patients, mocking and bullying people at their most vulnerable, swearing and humiliating the individuals they were supposed to be caring for. Concerns about failures by Greater Manchester Mental Health Service NHS Foundation Trust (GMMH), which runs the Edenfield Centre, had been reported by the Manchester Evening News in the years prior to the Edenfield abuse footage. But admissions to the centre were largely suspended after the Panorama episode, followed by a number of reports and investigations – until now.Yesterday, September 4, GMMH bosses told Manchester City Council’s health scrutiny committee that the Edenfield Centre would be reopening to patient admissions. “I’m really, really excited… we are so close now to agreeing with our commissioners that we can reopen the Edenfield Centre to admissions. We’ve got a very pivotal meeting tomorrow morning (August 5),” Fleur Bakeman, the improvement director at the mental health trust, told the committee. “I’m really, really crossing everything that we can get that over the line – for all sorts of reasons, but not least our service users so that we can accommodate our service users closer to home. From our staff perspective, to give them a real boost, that all the hard work they have been doing over the last 18 months is culminating in that.“But also for the city, really, it’s a really big bed base. At the moment, a lot of that is closed to admissions, so for me that was a big piece.” Source: Manchester Evening News, 5th September 2024
August 2024
‘I’ll knock him the f*** out’: Abusive mental health nurse threatened to ‘kill’ patient
Andrea Burdon unleashed a tirade of “vulgar” and “abusive” language on the vulnerable patient at the All Saints Hospital, a specialist mental health facility in Oldham
A mental health nurse who threatened to “knock out” a deaf patient has been banned from the profession.
Andrea Burdon unleashed a tirade of “vulgar” and “abusive” language on the vulnerable man while treating him at All Saints Hospital, a specialist mental health facility in Oldham. She lashed out at the patient after he refused to let her administer his medication, branding him a “fat b******”.
She has since been found no longer fit to practice by a Nursing and Midwifery Council (NMC) panel and has been struck off the nurses register. The panel heard that Ms Burdon had gone to check the patient’s blood glucose levels on May 5, 2020.
When he requested another nurse, Ms Burdon refused and grabbed the patient’s hand to carry out the test. The patient pulled their hand away and clenched their fist.
The panel heard that Ms Burdon then told him: “Go on then, f****** hit me, I will f****** hit you back”.
She then poked him in the shoulder, causing him to fall onto his bed. Ms Burdon then threatened to retaliate if the “distressed” patient attacked her.
Ms Burdon left the room but continued to shout at the man, who had been diagnosed with paranoid schizophrenia and a personality disorder. The panel heard that she threatened to “kill” the patient and said: “I’ll knock him the f*** out.”
A colleague witnessed the incident and reported it. Ms Burdon was suspended from her position before being dismissed in July 2020.
NHS 111 offering crisis mental health support for the first time
Millions of patients experiencing a mental health crisis can now benefit from support through 111, the NHS has announced today.
The change means the NHS in England is one of the first countries in the world to offer access to a 24/7 full package of mental health crisis support through one single phone line.
People of all ages, including children, who are in crisis or concerned family and loved ones can now call 111, select the mental health option and speak to a trained mental health professional.
NHS staff can guide callers with next steps such organising face-to-face community support or facilitating access to alternatives services, such as crisis cafés or safe havens which provide a place for people to stay as an alternative to A&E or a hospital admission.
Previously, local health systems had their own separate phone lines, which were fast-tracked during the pandemic and took around 200,000 calls per month.
More than 1,000 people in Greater Manchester were given ‘out-of-area’ hospital placements
Out-of-area placements happen because hospitals do not have enough beds for their patients. The 1000-plus patients from Greater Manchester who were sent to another county represent more than a fifth of the national total of out-of-area placements last year.
Some placements are at a relatively short distance, but most Greater Manchester patients were sent more than 62 miles (100km) away, at a total cost of £25.6m.
May 2024
GMMH Psychiatrist who cut monitoring frequency of patient before death ‘didn’t know 22-year-old was at A&E with self-harm injuries two days before’
Cerys Lupton-Jones was just 22 when she died following a stay at a Manchester mental health unit
A psychiatrist who reduced the amount an in-patient at a mental health unit was being observed in the week before her death has said he was not aware she was admitted to A&E with self harm related injuries less than 48 hours earlier.
Cerys Lupton-Jones was just 22 when she died following a stay of around six months in Park House, a mental health unit based at North Manchester General Hospital. The unit is operated by Greater Manchester Mental Health NHS Trust.
Cerys was found ‘unconscious’ on Elm ward on the afternoon of May 13, 2022. She died five days later. Cerys died with her family and friends at her side on May 18, after it became clear she would not regain consciousness and her life support was turned off, her family told the M.E.N.
A pre-inquest review into her death in October heard Cerys was involved in a ‘ligature event’ the previous day, May 12, and another at around 2.30pm on May 13.She was then found unconscious after another incident involving a ligature half an hour later, at around 3pm.
On Tuesday (May 7) an inquest at Manchester Coroner’s court, nearly two years after Cerys’ death, heard the 22-year-old had suffered ‘a number of deliberate self harm incidents’ and was detained under section 3 of the mental health act for treatment.
Parent’s heartbreak after ‘bubbly’ daughter found unresponsive in bedroom at mental health hospital just weeks into her stay
Leah Taylor, 20, was found unresponsive in her room at the Eleanor Hospital in West Didsbury last year
The parents of a woman who ‘brought light and laughter’ to the lives of all who knew her have told of the devastation of losing their daughter just weeks into her stay at a mental health hospital.
Leah Taylor, 20, from Urmston was admitted to Eleanor Hospital in West Didsbury on May 24 last year and detained under Section three of the Mental Health Act, a jury inquest into her death at Manchester Coroner’s Court heard.
Less than a month later, in the early hours of June 17, she was found unresponsive in her bedroom and tragically pronounced dead by paramedics. At the time Leah was being monitored four times an hour by staff.
On the first day of the inquest into her death on Monday (May 20) coroner Zak Golombeck told the jury that one of the issues he wanted the jury to focus on was whether Leah should have been placed on constant one-to-one observations in the period leading up to her death.
In a summary of the case he told the jury there had been ‘multiple incidents’ of deliberate self harm involving Leah during her stay at Eleanor Hospital, including eight incidents on the day before her death.
Eleanor hospital, run by Equilibrium Healthcare, provides care for women who have been diagnosed with a personality disorder or mental illness.
In 2022 Eleanor Hospital was rated ‘inadequate’ following an inspection by the Care Quality Commission (CQC) in May of that year and placed in special measures.
Inquest into death of 22-year-old woman who died at mental health unit adjourned while CPS investigate
Cerys Lupton-Jones died following a stay at a Manchester mental health unit
An inquest into the death of a 22-year-old woman who died after staying at a Greater Manchester mental health unit has been adjourned to allow the Crown Prosecution Service (CPS) to investigate – leaving her family waiting for answers nearly two years after her death.
The inquest into Cerys Lupton-Jones’ death began at Manchester Coroner’s Court on Tuesday (May 9) and was adjourned under coroner Zak Golombek the following day.
Evidence has been referred to the CPS to allow them to investigate and decide whether any criminal charges need to be brought.
April 2024
Greater Manchester’s NHS being plunged into ‘special measures’ over £180m black hole of debt
The region’s NHS has been reporting a deficit of around £180m for months (Image: NHS GM/MEN)
Greater Manchester’s health and care services, including the region’s NHS, have already been forced to massively cut an overspend of £400m over the last year. Accounting consultants were brought in to carry out a ‘financial turnaround programme’ during the first round of intense scrutiny from national NHS bosses. However, the system remains in hundreds of millions of pounds of debt – with a deficit of £180m.
A staff briefing from NHS Greater Manchester, seen by the M.E.N. this morning (April 25), says that it has ‘not yet been able to demonstrate to NHS England (NHSE) that we, as a system, have made the progress required against our well-publicised performance, finance and quality issues’. The city-region’s NHS will now have to go under the next level of scrutiny from its national governor, NHS England, and NHS England’s regional leaders.
The M.E.N. understands from a number of sources that these measures are the equivalent of going into a form of special measures for the region’s NHS system, and will likely be coming into force next month. NHS Greater Manchester has told the M.E.N. there are four levels of oversight by NHS England, with Greater Manchester now going into level three, ‘meaning NHSE regional team works with us to help us identify what is causing the key areas of concern and, between us, we agree an improvement plan with their support’.
However, NHS Greater Manchester says there is still one higher level of scrutiny could face, which they say replaced the formal special measures programme the NHS used to have. The fourth level is now referred to as the recovery support programme and is used to provide intensive support to failing organisations.
NHS Greater Manchester is being put on a ‘system improvement plan’, involving a set of ‘formalised agreed actions’ to be ‘delivered within a specific (yet to be determined) timeframe’.
The staff briefing reads: “NHS Greater Manchester (NHS GM) is still a relatively new organisation which continues to grow in maturity. Despite making good progress in embedding the operational plans which were designed in 2023 with the support of Carnall Farrar and Price Waterhouse Cooper; and despite the incredible hard work and effort that has happened over the last year to reduce our overspend from around £400m to £180m for 2023/24, we enter 2024/25 needing to address the most complex set of challenges that the health and care system in GM has ever faced.”
The region’s integrated care system (ICS) is responsible for paying for, planning and delivering Greater Manchester’s health and care needs, including most NHS services in the area. It is run by an integrated care board.
“Unfortunately, so far, the Integrated Care Board (ICB) has not yet been able to demonstrate to NHS England (NHSE) that we, as a system, have made the progress required against our well-publicised performance, finance and quality issues,” the staff briefing continues. “As a result of this, NHSE has indicated the ICB must work more closely with them to develop a set of formalised agreed actions under one single ‘system improvement plan’ to be delivered within a specific (yet to be determined) timeframe.
“An ICB programme team will be dedicated to delivering this plan, and overseen by a system improvement board (chaired by NHSE’s regional director). This is a process referred to legally as ‘Enforcement Undertakings’ and it is anticipated that this intervention will provide the regional team with a greater level of assurance on our progress.”
NHS England describes ‘enforcement undertakings’ as a level of enforcement action ‘where NHS England has reasonable grounds to suspect a potential failure or is concerned that an ICB is at risk of failing to discharge its function’.
Striking NHS junior doctors on the picket line outside Leicester Royal Infirmary
The region has blamed industrial actions costs as one of the reasons for the huge deficit (Image: Jacob King/PA Wire)
The M.E.N. has previously reported the financial turmoil of NHS Greater Manchester. Late last year, its debt spiralled by more than £800,000 a day in just four months, ending at the £180m deficit figure.
The region’s NHS said the reasons include ‘the ongoing impact of industrial action’ as NHS staff have been on strike for much of the last year, the cost of bank and agency staff needed to fill shortages, and the rising costs of both prescription drugs and ward beds for mental health patients. The regional organisation has been at that level of debt for months – all while trying to pay the regular bills for medical care and drugs being delivered across the 10 boroughs.
Last year, the growing shortfall prompted ‘additional scrutiny’ from NHS England. It was warned that the extra scrutiny could become full-scale intervention if Greater Manchester did not demonstrate ‘fundamental improvements’.
NHSE has placed NHS Greater Manchester into segment three of its standard operating framework, referred to as SOF 3. The framework reads: “For trusts and ICBs in segment three, NHS England and NHS Improvement regional teams will work collaboratively with them to undertake a diagnostic stocktake to identify the key drivers of the concerns that need to be resolved. Through this, we aim to better understand their support needs and agree improvement actions.”
There is still one further level of intervention, SOF 4, which NHS England says replaced the previous formalised financial and quality special measures programmes. SOF 4 provides the most intensive support to organisations ‘with the toughest challenges’.
What is the Greater Manchester Integrated Care System?
Integrated care systems (ICSs) are partnerships that bring together NHS organisations, local authorities and others to plan services, improve health and reduce inequalities. In Greater Manchester, the ICS provides health and care for a diverse population of approximately 3.1m people across 10 localities and 66 neighbourhoods, according to NHS England.
The ICSs are legally bound to plan and fund most NHS services in the areas they control – including NHS workforce planning. The systems are also required to bring together a broad range of organisations which have an influence on people’s health – including councils, voluntary groups, charities, and a host of NHS staff – to create a strategy to tackle public health and social care in each area.
Family of Manchester man killed by his cousin say he was let down by police and mental health team
The family of a man who was murdered by his mentally ill cousin say police and mental health services should have done more, after an inquest found their actions had “probably contributed” to his death.
Ryan Lowry, a tree surgeon and foster parent from Partington in Manchester, was struck 13 times with an axe by his cousin Ashley Glennon, a paranoid schizophrenic with a history of violence on 27 February 2020.
Ryan’s wife, Michelle, said: “Everything is different now, the whole world has changed. You lead completely different lives.”
An inquest at Stockport Coroners Court heard how he was under the care of the Greater Manchester Health Trust while also being supervised by Greater Manchester Police’s (GMP) Sexual Offender Management team.
Despite this, both organisations failed to share information on Glennon and missed several opportunities to prevent Ryan Lowry’s death.
Michelle said: “[Ashley] had several serious relapses of increasing levels of violence in the time coming up to it. The information was there, it just wasn’t acted on.
“The day before Ryan was killed, Glennon had smashed a window and kicked in a door at his ex-partners house.When Glennon’s ex-partner rang the police to tell them what happened, she was put on hold for 40 minutes before being disconnected.
Meanwhile Ryan, worried about his cousin’s mental state, had contacted his mental health team.They spoke to Glennon by phone, but failed to pass on any information to GMP.
Michelle said: “They didn’t ask him about the incident earlier in the day. He portrayed himself as being in a much better position than he was in.”
Ryan’s brother, Daniel, added: “There was just missed opportunities on all levels”
That evening, Ryan went to check on his cousin, who chased him out onto a street and killed him with an axe.Glennon, then aged 32, pleaded guilty to manslaughter by reason of diminished responsibility and was sentenced to an indefinite hospital order in January 2021.
Ryan’s family are being supported by Julian Hendy from the Hundred Families, a charity which provides information and practical advice for families bereaved by people with mental health problemsHe says this case is just the tip of the iceberg.
He said: “I’ve documented over 250 homicides by people with serious illnesses in the north west since 1993.
“Often it’s a failure to assess risk properly… These are people that can be dangerous when unwell or unmedicated and people often don’t appreciate that or act on what they know.”
Dr Arasu Kuppuswamy, Chief Medical Officer at Greater Manchester Mental Health NHS Foundation Trust said: “We express our deepest sympathies to Ryan Lowry’s family and friends following his tragic and untimely death.
“We are very sorry for the shortcomings in the standard of care and treatment we provided to Mr Glennon.
“Since Ryan Lowry’s death, the circumstances were thoroughly investigated both by GMMH, and by NHS England, who commissioned an independent investigation.
“In response to this, and as part of a wider initiative to improve our services for all our service users, carers and families, we have put a number of measures in place.
“This includes implementing a new Clinical Risk Assessment and Safety Plan Tool, which is being rolled out across the Trust following a successful pilot, supported by a comprehensive training package for staff.
“Every local Division at GMMH now also has its own dedicated Safeguarding Lead, to support and strengthen safeguarding.
“And we have reviewed and improved our Together Strategy, to make sure that service user and carer collaboration is at the heart of everything we do.
“We will continue to review this important work to ensure it is properly embedded and built upon where necessary.” In a statement, Greater Manchester Police said: “Our thoughts and condolences are with Mr Lowry’s family at this difficult time.
“We respect the findings of the Jury and acknowledge the comments made concerning the handling of the 101 call made in this case, and Greater Manchester Police’s Sex Offender Management Unit (SOMU).
“We recognise the importance of effective call handling and multi-agency information sharing and are committed to making further improvements in these areas to better serve and protect the public.
“Whilst of little consolation to Mr Lowry’s family, technical issues within GMP’s 101 system back in 2020 have been fixed, and calls to 101 now take on average 54 seconds to be answered.
“GMP’s SOMU has also made significant progress in reducing backlogs and improving the timeliness of offender visits.”
‘My Charlie lost his life while supposedly in a place he was being cared for – I will fight for justice’
Charlie Millers’ mum has vowed to continue her ‘fight for justice’ – and has called for a public inquiry into an NHS trust – after an inquest jury concluded he did not intend to take his own life and identified failings in his care.
The 17-year-old trans boy from Stretford, Trafford, died five days after he was found unresponsive in his room on mental health unit Junction 17, at the site of the former Prestwich Hospital, run by Greater Manchester Mental Health Trust (GMMH) late in the evening of December 2, 2020.
On Thursday (April 25), a jury said a lack of one-to-one, constant nursing care likely ‘contributed to his death’. Jurors determined Trafford council services did not communicate with each other effectively enough and did not provide Charlie’s mum the ‘practical support’ she needed as his mental health worsened, without enough help in the community.
They also said he should have been the subject of a ‘care protection plan’. Jurors said GMMH’s observation system, where staff checked on Charlie during his stays on wards including at the time he was fatally injured, was ‘not robust enough’ and was undertaken ‘inconsistently at best’.
GMMH said ‘a wide range of actions have already been taken to improve inpatient mental health services both in response to Charlie’s death, and as part of [a] wider improvement plan’.
The senior coroner who presided over the inquest, Joanne Kearsley, told jurors she would write to the Home Office, the Department for Health and Social care and agencies in Greater Manchester for their responses to the case, adding: “If there is going to be effective learning from these deaths, it must be done quickly.”
Following the hearing, Charlie’s mother Samantha told the Manchester Evening News: “I am shocked… in fact, beyond shocked. I will continue to push in every possible direction. I will look into the possibility of taking legal action against the trust and I want Greater Manchester Police to re-open their inquiry.
“The inquest heard there was insufficient evidence for them [GMP] to do a thorough investigation. I believe they should look at it again.
“I think the trust and Trafford council have failed. Given the fact there were three deaths of young people in nine months at the same site, we need to call for a public inquiry.”
Teenager with a ‘history of severe self-harm’ was told his life was a ‘car crash’ by psychiatrist before he died
Dr Akhtar Kapasi, labelled ‘Charlie or his life as a car crash’ while he was staying on the ward before having to apologise for using those terms. There were also incidents where staff and other patients would misgender Charlie, calling him ‘she’, with Samantha, the mother saying she felt ‘nothing really got done about it’ even though it caused Charlie to become upset.
Charlie Millers died aged 17 after staying on at Junction 17 on Greater Manchester Mental Health Trust’s Prestwich site (Image: MEN Media)
A teenager with a ‘history of severe self-harm’ was told his life was a ‘car crash’ by a psychiatrist involved in his care in a ‘stretched’ mental health unit, an inquest has heard.
The inquest into the death of Charlie Millers has started after more than a year of delays. The 17-year-old trans boy died five days after he was found unresponsive in his room on mental health unit Junction 17 at the former Prestwich Hospital site, run by Greater Manchester Mental Health Trust (GMMH), on December 2, 2020.
Two other patients being treated at the hospital also died within nine months of Charlie.
The first day of the four-week inquest was told how Charlie had been through a lot of ‘trauma’ throughout his life including being ‘bullied at school’, with ‘acid thrown on him’ and ‘sexual abuse’ over the course of five years. Charlie felt ‘worthless’, struggled with ‘big feelings of shame’, and ‘did not feel safe in his relationships’ ahead of his death, one doctor said.
An inquest into the death of Charlie was delayed in January 2023 so the Greater Manchester Police inquiry could take place after it emerged at a coronial hearing that hospital records may have been edited after his death.
The Manchester Evening News understands a GMP investigation has concluded and that there is insufficient evidence for authorities to seek a prosecution for manslaughter by gross negligence. The inquest into Charlie’s death began today, April 8, at Rochdale Coroner’s Court.
Charlie died from a hypoxic brain injury after being found completely unconscious with injuries caused by a ligature. At the time, he was on a strict observation regime where he was supposed to be checked on every five minutes, heard the court.
Charlie, from Old Trafford, had struggled with his mental health from around the age of five which worsened throughout his teenage years. Those struggles included serious self-harm, thoughts of wanting to die, and hearing voices including a voice which Charlie named ‘X’, which told him to harm his family or himself.
The voice would threaten that ‘bad things would happen to him or his family’, playing into Charlie’s fears of those close to him being hurt as he ‘loved his family so much’.
“There was always the risk that we could find him not alive and his siblings were well aware of that as well. They were worried what they’d find at home,” Samantha said.Despite the strain on the family, mum Samantha was determined to make sure Charlie got help. She said that included supporting Charlie in exploring his gender dysphoria, as Charlie had been saying from a young age while still at primary school, ‘I am a boy’.
Charlie wanted to pursue medical intervention including starting puberty suppressing hormones. His family and school helped him with a referral to the Gender Identity Service (GIDS) for young people run by Tavistock and Portman NHS Trust, where he had been undergoing assessment.
The court heard from the former head of the now-closed service, Dr Polly Carmichael, who said that Charlie’s mental health was never determined as stable enough for him to go on to a ‘medical pathway’ which would have seen him be provided with the hormones.
Charlie struggled with his mental health from a young age, and suffered severe self-harm and suicidal thoughts (Image: Collect unknown)
Samantha also supported Charlie as he began a damaging cycle of coming in and out of hospital as his mental health spiralled, the court heard. He was too unstable to remain at home, but being on loud and disruptive mental health wards was also ‘causing harm’ to Charlie, who had an ADHD diagnosis and documented features of autism spectrum disorder, and needed routine, according to his mum and one of Charlie’s psychologists on Junction 17.
Dr Laura Ecclestone told the court that staffing was stretched on the ward, saying: “I wanted to do more for every young person on that ward. I was stretched, and it was hard… it was a hard year.”
She said she has been traumatised by Charlie’s death and ‘giving so much of herself’ during a difficult period for the ward and GMMH.
“No one wants a child to be in an in-patient setting… In some ways it was causing harm for Charlie,” she added.Samantha Millers said Charlie did have good relationships with some staff on the ward, but told the court how a psychiatrist,
Mental health trust investigation into Charlie Millers’ death was ‘lacking’
‘The outcome of the 2020 investigation is that the ward was adequately staffed, but you didn’t speak to all of the staff?’, the coroner questioned
Greater Manchester Mental Health Trust’s (GMMH) investigation into the death of Charlie Millers has been described as ‘lacking’ after bosses failed to speak to all staff members working on the ward at the time when the teenager was fatally injured there.
The 17-year-old trans boy died five days after he was found unresponsive in his room on mental health unit Junction 17 at the site of the former Prestwich Hospital, run by Greater Manchester Mental Health Trust (GMMH) late in the evening of December 2, 2020.
Mental health unit managers were also told to audit observations being done on patients staying on wards after fears they were not being done – only for those audits to also go uncompleted, an inquest has heard. GMMH managers were instructed to carry out daily audits of the regular checks being carried out on patients by ward staff.
The audit programme followed concerns in October 2020 that those regular checks, where patients are observed a set number of times an hour in accordance with their condition, were not accurate or simply not being done. But it was later found that the ‘there was no evidence’ some of the audits themselves were ever done.
Charlie Millers inquest: Son’s mental health support was a mess – mum
The mother of a teenager who took his own life while he was a patient at a secure mental health hospital has told an inquest his support “was a mess”.
Charlie Millers, 17, was a patient at Greater Manchester Mental Health Trust’s Prestwich Hospital in 2020.
His mother told the inquest there was conflict between social workers and the hospital’s Junction 17 unit and she felt “nothing was getting sorted out”.
Charlie was one of three people who died in less than a year at the site.
The deaths of Rowan Thompson, 18, Ania Sohail, 21, and Charlie, from Stretford, Greater Manchester, took place in a nine month period between October 2020 and June 2021.
Charlie’s inquest was adjourned in 2023 after police announced they had started a manslaughter investigation.
The investigation concluded with a decision not to prosecute in January.
March 2024
Gaynor Chapman, 53, from Salford, was found dead at Park House
Heartbroken family pay tribute to mum with the ‘kindest heart’ found dead at mental health hospital
Gaynor Chapman, 53, from Salford, died last Friday (March 1) – the day after she had first attended the Park House a GMMH mental health hospital, in Crumpsall.
Her niece Shelby has told the Manchester Evening News that Gaynor had been admitted the day before her body was found. The police were called to the scene, and the NHS trust have said they are cooperating with the investigation.
The mum-of-two, who lost her son Zane when he was just 27-years-old in 2018, had struggled with her own mental health following his death, Shelby said.
Gaynor, who was a grandmother-to-four, was described as having ‘the kindest heart’ who ‘loved her family, loved animals and her grandchildren’.
Shelby said: “She had the kindest heart. If you had any problems, she would always be the first to be there for everyone. She was bright and bubbly. Her whole life was her family and her grandchildren. Church was also a huge part of her life which helped her through difficult times. “Everyone in the family has been coming together, and it has shown how loved she truly was and how many people cared about her. She was definitely loved.
“[Her death] has just ripped everybody’s heart out. It was so unexpected – all she did was ask for help.”
It is understood Greater Manchester Police are carrying out a special procedure investigation into Gaynor’s death. The force confirmed they were called to the scene on the evening of March 1.
The Greater Manchester Mental Health NHS Foundation Trust (GMMH), which operates the hospital, has confirmed it is cooperating with police investigations. Manchester coroner’s office has confirmed that Gaynor’s death has been referred to them.
Dr Arasu Kuppuswamy, Chief Medical Officer at Greater Manchester Mental Health NHS Foundation Trust said: “We can confirm that an incident occurred at Park House on 01 March 2024. We are cooperating fully with GMP’s investigation. Our thoughts remain with everyone who has been affected at this difficult time.”
11.14pm, 11.16pm, 11.17pm, 11.26pm, 11.43pm… the unanswered calls of a desperate woman: Madeline Hughes needed help, but nobody picked up the phone
A personal trainer with a history of mental health problems took her own life following a series of unanswered calls to a helpline, an inquest heard. Madeline Hughes, 34, suffered catastrophic fatal injuries after deliberately walking into the path of a train. Ms Hughes was at home in south Manchester when she made five calls to the Laureate House ‘home-based treatment team’ – on the grounds of Wythenshawe Hospital, run by Greater Manchester Mental Health NHS Foundation Trust – just before midnight on April 21.
None of the calls were picked up, an inquest into Ms Hughes’ death was told. She became ‘agitated’, before her mother called 999 when her daughter ‘sprinted’ out of the house in Northenden.
As a search began, Ms Hughes managed to climb onto a railway line off a motorway, before crouching in front of a speeding train. She died at the scene.
An inquest at Manchester Coroners’ Court on Tuesday (March 26) heard Ms Hughes had struggled with mental health problems from 2009 and that her condition worsened during the pandemic. She sought help privately from The Priory and via her GP, who referred her to Greater Manchester Mental Health NHS Foundation Trust, the court was told.
She was diagnosed with bipolar affective disorder and ADHD. Ms Hughes was prescribed an anti-psychotic medication quetiapine for bipolar disorder, but when it caused her muscle stiffness, it was replaced by another drug, ariprazole.
By the time of her death, this was in the process of being replaced by a third drug, lamotrigine, the inquest heard. She was also prescribed, but was wary of taking and becoming addicted to, anti-depressant diazepam. The inquest heard Ms Hughes had pressed for medication for her ADHD, but was told that had to wait until her bipolar disorder was under control.
Ms Hughes made her calls to the ‘home-based treatment team’ (HBMHT) at 11.14pm, 11.16pm, 11.17pm, 11.26pm and 11.43pm, but an investigation failed to establish why the lone night-shift worker on duty that night night didn’t answer the calls. The inquest heard there were signal blackspots at Wythenshawe Hospital. She was hit by the train at around midnight.
New community mental health service to roll out in Wigan following successful pilot
A new trauma informed community mental health service is being rolled out to other parts of Wigan following a successful pilot.
And those who have themselves battled mental health issues play a key role in its success
Wigan Borough Living Well has seen Greater Manchester Mental Health NHS Foundation Trust (GMMH) join forces with Wigan Primary Care, Wigan and Leigh Community Charity, and Wigan Council.
The service – part of the national Living Well programme – is funded by Greater Manchester Integrated Care Partnership and supported by the Innovation Unit.
It will support people who are experiencing mental health problems, by understanding their goals and working with them to achieve them in a holistic way.
Alongside dedicated mental health support and treatment from NHS clinicians, the service will also connect people with their local community, and help them in other areas of their lives which they may need support with – and which might also be having an impact on their mental health – including housing, employment, loneliness, debt, or substance misuse.
The service will take a “trauma-informed” approach to care, meaning that it will seek to understand past traumatic events people may have experienced how this may have had a lasting impact on their wellbeing, and what they may need to help them move forward.
February 2024
Plagued by safety fears, Greater Manchester Mental Health Trust, our biggest mental health service has had another terrible report
One ward inspected was found to be ‘not fit for purpose’, according to latest findings.Another report has been published. Greater Manchester’s biggest mental health service is still plagued by safety fears, with buildings that ‘do not protect the dignity, privacy and safety of patients’, inspectors have again found. The region’s largest mental health provider has been under scrutiny for almost 18 months after a host of failings to the most vulnerable patients came to light.
Care Quality Commission (CQC) inspectors rated Greater Manchester Mental Health Trust (GMMH) ‘inadequate’ following an inspection in 2023. Months later, in June last year, the watchdog again carried out an unannounced inspection after receiving information on concerns about the ‘safety and quality of services’. The latest findings were published today (Tuesday, February 7). Inspectors said psychiatric wards and intensive care units still have safeguarding problems; almost half of staff remain untrained in some key areas on one ward; and actions have not been taken to tackle safeguarding incidents.
Patients themselves gave mixed feedback about their experiences of care and treatment on the wards. Patients said they ‘generally felt safe on the wards and those that did not reported that this was often due to other patients’ behaviour or the general acuity of the ward’. However, patients were concerned ‘about the high levels of bank and agency staff used on the wards and that the quality of care these staff delivered could differ significantly’, the report said, adding: “Patients felt that non-permanent staff were less caring and less interested in supporting patients on the ward.”
Police probe continuing into alleged mistreatment of patients at under-fire mental health trust unit
Three members of staff are still being investigated, while 32 have ben told no further action will be taken against them. A police probe into the alleged mistreatment of patients at a unit run by under-fire Greater Manchester Mental Health Trust is ongoing, the Manchester Evening News has learned. Three staff remain under investigation by Greater Manchester Police, while 32 others have been told they face no further action.
Mental health trust denied patients ‘basic dignity and human rights’
Mental health trust denied patients ‘basic dignity and human rights’, prioritised white people and fostered ‘culture of fear and intimidation’ despite extra scrutiny after being exposed by Panorama investigation in 2022. A review into a mental health trust found patients were denied ‘basic dignity and human rights’ and staff were afraid to speak out in a culture of ‘fear and intimidation’. The independent report into Edenfield Centre, near Manchester, also found that patients who were white were ‘prioritised’ and ethnic minority staff members at the Trust felt there was ‘no point’ in applying for promotion
Independent report into abuses at GMMH published – see main findings and recommendations
Here is a useful summary from the BBC of the main findings of the recently published independent report into GMMH and Edenfield. The report outlines a series of recommendations for the trust, which include ensuring patient, family and staff voices are heard “at every level” and creating a culture where quality of care is the “utmost priority”. Other recommendations include a call to adapt to problems caused by staff shortages, to address the poor state of some building, and for a review into oversight to “prevent tragedies like those seen at Edenfield from reoccurring”. The independent report, led by Prof Oliver Shanley OBE, found the trust repeatedly missed opportunities to act on concerns, alongside a culture of “suppressing bad news”. It found the Panorama broadcast exposed the “most shocking abuse and poor care” of vulnerable patients, and that concerns raised by families were “not always taken seriously”. It added that in some services, patients had been denied “basic dignity and their human rights”
January 2024
Manchester leaders have again slammed the failing mental health trust after months of promised improvements – to little avail. More than half of Manchester mental health patients are not being read their rights within two weeks of being sectioned. Just 47 per cent of patients in south Manchester and only 41 per cent of patients in north Manchester are being read their rights within the first two weeks of admission to hospital after being detained under the Mental Health Act, also known as being sectioned. The Manchester Evening News can reveal the shocking data after it was aired in a small council meeting to monitor Greater Manchester Mental Health Trust’s (GMMH) performance after more than a year of revelations about patient abuse, neglect and failure of patients.
December 2023
Mental health bosses can’t say whether disgusting patient abuse uncovered in Greater Manchester hospital is still happening
Some staff were filmed by an undercover Panorama reporter embedded in the unit, the footage appeared to show patients being bullied, humiliated, swore at and taunted. Mental health bosses could not say whether the kind of abuse uncovered in one in-patient psychiatric facility is still happening across Greater Manchester’s mental health services.
Greater Manchester Mental Health Trust apology after Horwich death
A 75-year-old man with depression was discovered dead after the NHS Trust responsible for his treatment missed up to five visits. There was “no continuity of care”. Robert Leigh, from Horwich, was discovered dead at his home this year in what coroner Professor Dr Alan Walsh ruled as a suicide.
Nearly a third of staff absences in the Greater Manchester Mental Health Trust are stress-related
Nearly a third of staff absences in the Greater Manchester Mental Health Trust over the past year were stress-related, new figures show.Health think tank The King’s Fund said staff shortages across the NHS must be addressed to ease stress and heavy workloads. NHS Digital figures show there were roughly 48,500 full-time equivalent days lost due to stress-related absences in the year to June at Greater Manchester Mental Health NHS Foundation Trust – accounting for 32.9% of the total 147,200 days lost. It is up from 32.2% of staff absences in 2021-22. The figures cover all professionally qualified clinical staff, clinical support staff, and infrastructure support staff who were absent due to anxiety, stress, depression or other psychiatric illnesses.
Almost 15,000 Manchester children in contact with mental health services
Almost 15,000 children in Manchester were in contact with mental health services in the year to September, new figures show.It comes as more children than ever accessed mental health services across England, with the number of open referrals having almost doubled throughout the coronavirus pandemic.Mental health charity YoungMinds said the Government is failing to take action against a “deepening” crisis.NHS Digital figures show around 14,800 children in the former NHS Manchester CCG area were in contact with mental health services in the year to September.
November 2023
Greater Manchester mental health service under ‘sustained pressure’
Mental health services across Greater Manchester are coming under “sustained pressure” due to a £90m shortfall in investment, a watchdog has found. The city region’s Integrated Care Board, which reviews how NHS cash is spent, said mental health provision had levels of investment below the national average. The board said “fundamental changes” were needed. Greater Manchester Mental Health Trust said it was making improvements. The board’s findings, reported by the Local Democracy Reporting Service, come after the trust was issued with a Section 29A warning notice by the Care Quality Commission in April 2022, which deemed it inadequate following an inspection.
Mental health services in the city region are suffering from a chronic shortfall in investment compared to elsewhere in the UK
Mental health services across Greater Manchester are suffering from £90 million of under-investment, according to a shocking report. The revelation follows an ‘independent diagnostic’ commissioned by Greater Manchester Integrated Care Board, which concluded the huge shortfall compared to elsewhere in the UK.
Priory Mental health hospital group that owns Cheadle Royal faces criminal charges over patient killed by train
Matthew Caseby, who was left unattended for more than six minutes before absconding from Priory Hospital Woodbourne in Birmingham, an inquest heard. The Priory mental health hospital group has been has been charged with exposing a patient to a significant risk of avoidable harm after a vulnerable man was killed by a train after absconding from a mental health hospital.
Tormented mental health nurse found dead following stay at GMMHT psychiatric hospital ‘We tried our absolute darnedest to make people listen and we were not heard’
A mental health nurse tormented by her sister’s death was found dead at home following a stay at a psychiatric hospital, an inquest heard. Natalie Cunliffe’s loved ones – devastated after her sibling took her own life – told a coroner their concerns were not ‘taken seriously’ by staff during her treatment.
‘GMMH should be screaming from the rooftops’: Our mental health service needs £90m now
Senior councillors message to health bosses “What kind of loud noise is being made about being under-provided with cash in Greater Manchester in comparison with other areas and shouldn’t people in the health service and politics be screaming from the rooftops about it? If not, why aren’t they? Because I’m sure that resonates with people.”
October 2023
Family of a man who took his own life at GMMHT psychiatric hospital brand failings as a ‘disgrace’
The family of a man who took his own life while in the care of a psychiatric hospital have branded failings in his treatment as a “disgrace”. Dad-of-two Niall Tyrell had been under 24-hour observations, but a failure in communication meant after being transferred to another ward, he was only checked every 15 minutes. It was during one of those breaks he tried to take his own life and was found unresponsive in his bedroom, in Park House, in the grounds of North Manchester General Hospital. Greater Manchester Mental Health Trust, which runs the unit and is currently rated as inadequate by the Care Quality Commission, admitted to failings at Niall’s inquests.
Priory Mental health hospital group that owns Cheadle Royal faces criminal charges over patient killed by train
Matthew Caseby, who was left unattended for more than six minutes before absconding from Priory Hospital Woodbourne in Birmingham, an inquest heard. The Priory mental health hospital group has been has been charged with exposing a patient to a significant risk of avoidable harm after a vulnerable man was killed by a train after absconding from a mental health hospital.
Tormented mental health nurse found dead following stay at GMMHT psychiatric hospital ‘We tried our absolute darnedest to make people listen and we were not heard’
A mental health nurse tormented by her sister’s death was found dead at home following a stay at a psychiatric hospital, an inquest heard. Natalie Cunliffe’s loved ones – devastated after her sibling took her own life – told a coroner their concerns were not ‘taken seriously’ by staff during her treatment. Mum-of-two Ms Cunliffe, described as ‘beautiful inside and out’, was found hanged at her home in Tyldesley, Wigan, on February 6. She was 29. An inquest into her death – attended by her parents, sibling and partner – at BoltonCoroners’ Court examined her care by mental health medics prior to her death.
Priory Cheadle Royal mental health hospital – where three young woman died within eight weeks – ordered to make improvements by watchdog after critical inspection report
A mental health hospital where three women died within eight weeks has been criticised by the health watchdog and issued a notice ordering bosses to make improvements. The Care Quality Commission (CQC) said changes need to be made on acute wards for adults, and on psychiatric intensive care units, at the Cheadle Royal Hospital, also known as The Priory.
Greater Mental Health Trust and Trafford Council rapped over £8K bill which caused ‘avoidable distress and worry’ Ombudsman critical of NHS trust and council over £8K bill which caused ‘avoidable distress and worry’
Mental health and town hall bosses rapped over £8K bill which caused ‘avoidable distress and worry’. Mental health and town hall bosses have been rapped for causing a man and his family eight months of ‘avoidable distress and worry ’ over an £8,000 bill for supported living they had not been warned about. Although the bill was eventually waived, the Local Government and Social Care Ombudsman has criticised Greater Manchester Mental Health NHS Foundation Trust – acting on behalf of Trafford council – about the way the man’s discharge from hospital was handled.
July 2023
Staff faced racism at yet another of GMMH troubled mental health units, review finds
Staff fear racism from fellow colleagues as well as patients – and worry there will be no action taken or even retribution after speaking up “This review focused on Park House; however, we know that people in other areas report the same experiences…”
Park House is a mental health unit at North Manchester General Hospital, run by the troubled Greater Manchester Mental Health NHS Foundation Trust (GMMH). The unit was investigated amid concerns about its culture, treatment and discriminatory practices affecting staff.
The review, carried out by GMMH, found racism was ‘present within cultural and social structures, systems and within our organisation’. Ethnically-diverse staff were found to have felt unsafe because of ‘racial abuse from patients and that abuse has not been dealt with effectively resulting in loss of faith in the system’.
June 2023
Greater Manchester Mental Health NHS Foundation Trust has been criticised in an independent investigation into the care and treatment of Ashley Rowen
Mental health staff did not effectively act upon a man’s grave concerns reported to them about his severely unwell cousin – hours before he was brutally murdered by him. Mental health staff caring for Rowen did not ‘adequately reflect and/or assess either his historic or most recent risk incidents’ – which included attacking his elderly grandfather, a domestic violence conviction, and threatening his own mother while in possession of a knife, the report says.
The NHS has published an independent investigation into the care and treatment of Ashley Rowen, also known as Ashley Glennon, by Greater Manchester Mental Health NHS Foundation Trust (GMMH). The mentally ill Rowen chased his cousin and main carer, Ryan Lowry, down the street and struck him 13 times with an axe in Partington on February 27, 2020.
‘Muddle, frustration and distrust’ at ‘most mature’ Greater Manchester Integrated Care System
Multiple problems have been highlighted with the leadership and governance of a much-vaunted integrated care system, including a lack of trust between organisations which often hide information that could weaken their position.
HSJ has seen an executive summary of the review of Greater Manchester ICS, which cited widespread concerns around the allocation of resources, confusion about the role of commissioning, and “muddled” governance.
It was conducted by consultancy firm Carnall Farrar, which held interviews and forums with more than 200 leaders in the system.
Black patients in Greater Manchester more than three times as likely as white patients to be detained
Black patients in Greater Manchester were more than three times as likely as white patients to be detained under the Mental Health Act last year, new figures show.
NHS England figures show about 2,255 white patients were detained in NHS Greater Manchester Integrated Care Board’s area the year to March 2022, while 285 patients detained were black or black British.
However, the rate of detentions when taking population size into account was higher for black patients, at 318 per 100,000 people compared to 98 per 100,000 for those that identified as white.
It meant black patients were 3.2 times as likely to be subject to a mental health detention in 2021-22. Jabeer Butt, CEO of the Race Equality Foundation, said the figures are “not new or surprising. The real question is why has this not changed, despite being well documented over a number of years, not just with these new figures. The health and care system fails to invest in early intervention even though this has been highlighted as an issue for a long time,” she said.
May 2023
High Court Application For Judicial Review Over Failure To Involve Service Users In Plans To Change Community Mental Health Services Across Greater Manchester
Public Law And Human Rights Lawyers Instructed By Service User To Issue Legal Challenge Into NHS Trust’s “Ongoing Failure” To Involve Public In Planning Process
‘I was forcibly restrained and injected with medication I didn’t want for months’ – They were at their lowest and this is how they were treated
Helena Vesty reports the latest in the Greater Manchester Mental Health Trust saga – as those needing help most speak of feeling abandoned by those supposed to be looking after them and being ‘shipped’ to distant parts of the country in their most distressing days.
GMMH publish Draft Improvement Plan to address Edenfield scandal and other service failings
This improvement journey will only succeed if the views of our service users, their families and carers, alongside those of our staff and stakeholders, are central to the development and implementation of our detailed plans.
The system is failing and these people deserved so much more
Manchester Evening News look at the fall of Greater Manchester’s Mental Health Trust – they ask what went wrong and why are many of the board members who presided over the failures listed in this piece are still leading the trust?
April 2023
Neil Thwaite, CEO of GMMH NHS Trust which runs Edenfield Centre to resign
Neil Thwaite, the CEO of GMMH NHS Trust in charge of the mental health unit in Prestwich at the centre of an undercover Panorama probe is set to step down from his role.
March 2023
GMMH pilot project to reduce reliance on mental health services and promote eventual independence set for expansion following initial success
A pilot mental health service in the north west could be set for an expansion after its first eight months was heralded a success. The service comes in the form of the Home Engagement and Rehabilitation Team (HEART) at Greater Manchester Mental Health NHS Foundation Trust (GMMH) which was set up to reduce reliance on mental health services and promote eventual independence.
NHS England accused of ‘massive betrayal’ over police-led SIM scheme
A policy to protect patients from the controversial SIM scheme has been indefinitely delayed NHS England has been accused by campaigners of a “massive betrayal” as it appeared to shelve a long-awaited policy to safeguard mental health patients accessing emergency care. The SIM scheme sees police embedded in clinical teams to help manage patients who persistently call emergency services.
NHS staff morale at the Greater Manchester Mental Health Trust at record low
Morale amongst staff at the Greater Manchester Mental Health Trust is at a record low, new figures show. Morale among staff was scored at 5.5 out of 10 in autumn 2022 – down from 5.8 the year before and the lowest since comparable records began in 2018.
CQC tells Greater Manchester Mental Health Trust to make further improvement
The Care Quality Commission (CQC) has told Greater Manchester Mental Health NHS Foundation Trust it must make improvements following an inspection of their community-based mental health services for people of working age in October.
GMMH publish Draft Improvement Plan to address Edenfield scandal and other service failings
“This improvement journey will only succeed if the views of our service users, their families and carers, alongside those of our staff and stakeholders, are central to the development and implementation of our detailed plans.”
‘We saw staff laughing at the people they were supposed to be looking after’
Inspectors found ‘disproportionate levels of restraint’, ‘care plans not being followed’, ‘people spending most of their time along in their rooms’. The Breightmet Centre for Autism in Bolton has been deemed ‘inadequate’ for a second consecutive time by health watchdog the Care Quality Commission (CQC). A damming report has now been released.
February 2023
Police in England and Wales dealing with more mental health crises than ever. Forces say increase highlights erosion of mental health services in recent years
The police are dealing with increasing demands to intervene with people suffering mental health crises, freedom of information requests have revealed. Some forces across England and Wales have experienced a tripling in mental health requests between 2019 and 2021, data shows.
Scandal-rocked Greater Manchester Mental Health Services hit with ‘inadequate’ rating as hospital wards branded unsafe
GMMH Trust has already been the subject of multiple investigations, the highest level of scrutiny from NHS England and being placed ‘in the equivalent of special measures’ Greater Manchester’s scandal-hit mental health services have been served with another warning notice to improve after inspectors found wards for older people were unsafe.
Almost 2,000 face long waits for mental health treatment in Manchester
Almost 2,000 people waited more than three months for a second mental health treatment in Manchester last year, figures show. As of November, around 4,315 people were waiting for a first treatment in Manchester. The findings come as a leading staff body for the profession says it is “unacceptable” so many are suffering delays
Bournemouth woman who died after being”left alone, far from home with no treatment” at Priory Hospital in Stockport was failed by mental health system, inquest told
Lauren Bridges was “left alone, far from home with no treatment”, her mother said. Lauren who was autistic, died while she was detained at Priory psychiatric hospital in Stockport, 250 miles (400 km) from her home. She was “massively failed by the mental health system”, an inquest jury has heard.
Bolton Hospital’s A&E gets important warning about mental health patients
However the A&E received praised for having competent staff, an effective leadership team, and treated patients with respect and kindness. The rating for safe in the emergency department has moved down from good to requires improvement amid concerns that people attending with mental ill health often experienced long delays in being assessed.
Professor Oliver Shanley appointed as Independent Chair of the Independent Review of GMMH Services
In November 2022, NHS England (NHSE) placed GMMH into NHS Oversight Framework (OF) segment 4 and enrolling the Trust into the Recovery Support Programme. At the same time, NHSE advised GMMH that they planned to commission an independent review into the Trust’s services.
January 2023
Record number of Greater Manchester Mental Health Trust staff resigned last year
A record number of staff left their posts at the Greater Manchester Mental Health Trust last year, new figures show. NHS Digital figures, which are rounded to the nearest five, show around 800 NHS staff resigned from their roles at Greater Manchester Mental Health NHS Foundation Trust in 2021-22.
Death of ‘caring’ young woman at GMMH mental health unit contributed to by ‘ineffective’ policies, inquest concludes
Ania Sohail, 22, collapsed after ingesting medication bought online whilst a patient at the Junction 17 unit in Prestwich The death of a “kind” and “caring” young woman at a mental health unit in Bury was contributed to by “ineffective” policies in place at the time, an inquest jury have concluded.
GMMH NHS trust investigated over alleged potential edits to records after death of patient
NHS trust investigated over alleged potential edits to records after death of patient Charlie Millers, 17, was found dead in his room at Prestwich mental health hospital in December 2020. The charity Inquest, which is supporting Millers’ family, described the new evidence as “deeply concerning”.
Ministers order ‘rapid review’ into mental health inpatient care in England
Dr Geraldine Strathdee to investigate care units after series of scandals involving abuse or neglect of vulnerable patients in psychiatric in-patient services Denis Campbell Ministers have ordered an inquiry into the quality of care in mental health inpatient units in England after a series of scandals in which vulnerable patients were abused or neglected.
December 2022
Dainius Pūras, psychiatrist, former UN Special Rapporteur on Human Rights and Mental Health
Dainius Pūras, psychiatrist, former UN Special Rapporteur on Human Rights and Mental Health speaks about the predominant importance of human rights in shifting the thinking and practice of bio-medical psychiatry across the world and in Manchester.
Bill McCarthy, former NHS boss to take over scandal-hit Greater Manchester mental health services
Bill McCarthy, a former NHS director has been revealed as the new chair of Greater Manchester Mental Health NHS Foundation Trust (GMMH). The appointment follows after ‘inexcusable behaviour and examples of unacceptable care’ were ‘exposed’ at a mental health unit, said the outgoing chair.
The mental health patients dying on GMMH NHS wards from neglect
Investigation: Scores of patients in mental health units have died from physical illnesses that could have been avoided. Rebecca Thomas uncovers systemic issues in the health service that experts say are leading to the neglect of the vulnerable.
Yvonne Eaves died from a blood clot while an inpatient at the Greater Manchester Mental Health NHS Foundation Trust in 2020, after staff within the unit failed to carry out a risk assessment for blood clots.
Great Manchester coroner Nigel Meadows attributed her death to “a gross failure to provide her with basic medical care”. Hers is one of four cases in which coroners warned of inadequate blood clot assessment and treatment within inpatient units.
Gill Green, of the Greater Manchester Mental Health NHS Foundation Trust, said improvements had been made to physical healthcare provision, including a new strategy and the introduction of new job roles with a physical healthcare focus.
‘Staggering’ rise in restraint of black people in mental healthcare
- Figures show steep rise in rates of black people receiving restrictive interventions
- Rates double in six years, but up 30 per cent for white people in same period
- Charities “appalled”, warning that data “reinforces impact of systemic racism” on safety
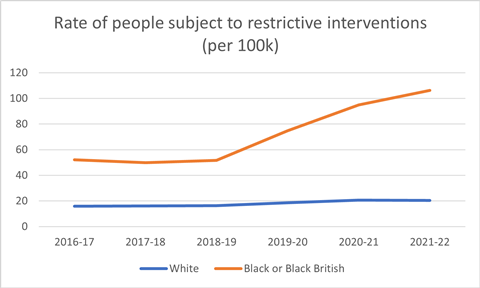
Dad struggling with his mental health died hours after asking hospital staff for a bed
A dad who asked for a bed at mental health hospital in Wigan, Greater Manchester, died hours after being told he would not be admitted, an inquest heard. Darren McHugh, 39, told mental health professionals he was hearing voices, felt paranoid and wanted to be treated on a mental health ward.
Coroner asks GMMH “Is it ever appropriate to tell a patient ‘we will see you tomorrow’ if a referral had not been made?
Daniel Kirton tragically died following the collision, which came after he had attempted to take his own life on hospital grounds following his discharge by mental health practitioners. He had attended Manchester Royal Infirmary’s emergency department earlier that afternoon, December 3, 2020, and was assessed by staff from the Greater Manchester Mental Health NHS Foundation Trust
November 2022
Charm’s response to the placing of Greater Manchester Mental Health Trust in ‘intensive care’ by NHS
Concerns raised by CHARM, service users, their families, and staff, some of which have been presented through the media have led to NHS England commissioning an independent review into the services provided by GMMH. The Trust has also been placed in ‘intensive care’ through the NHS Recovery Support Programme. Yesterday the CQC also told Greater Manchester Mental Health NHS Foundation Trust to make significant improvements and have suspended their rating. Given these circumstance we call for roots and branch review of mental health support of people in crisis across Greater Manchester.
Greater Manchester Mental Health Trust put on ‘highest level of intervention’ by NHS
Greater Manchester Mental Health trust is now under the highest level of NHS England scrutiny, the M.E.N. can confirm, following allegations that patients were abused. Greater Manchester’s mental health trust has been placed into the ‘equivalent of special measures’, the Manchester Evening News can reveal. The crisis measures enforced by the NHS come after allegations that patients were abused at a mental health unit run by the beleaguered trust.
Greater Manchester NHS mental health trust ordered to improve
Warning notices were served after the Care Quality Commission (CQC) inspected the Greater Manchester Mental Health NHS Foundation Trust (GMMH). On Wednesday the trust was told it would face the highest level of intervention from NHS England.
The trust said improvement work was already under way.
Law firm to investigate if senior managers were to blame for alleged abuse of patients at Edenfield mental health unit
The purpose of this investigation is to ascertain whether any individual or individuals employed by the GMMH Trust in a leadership capacity have caused or contributed towards failings in patient care’
Rupert Nichols, the chairman of the Greater Manchester Mental Health NHS Foundation Trust, which runs the unit has commissioned a law firm to carry out an “independent investigation”. It will scrutinise the role of the executive team, including the Chief Executive Officer, and the heads of specialist services including Edenfield management.
Chair of Greater Manchester Mental Health Trust to step down
The move comes after ‘inexcusable behaviour and examples of unacceptable care’ were ‘exposed’ at a mental health unit, he said
Rupert Nichols, chair of Greater Manchester Mental Health NHS Foundation Trust, wrote a letter to the governors, board members and colleagues at the trust, shared this afternoon (November 18). Although Mr Nichols’ term of office ends next July, he announced he would be ‘retiring’ early from the position at the end of December 2022.
A dozen staff sacked after allegations patients were abused in GMMH mental health unit
Thirty staff are the subject of disciplinary action after claims in a BBC Panorama programme that patients were abused at an NHS mental health unit. A dozen have been sacked, the MEN undertands, and another 18 are to face hearings.
Chair of GMMH , Rupert Nichols, formally apologised on behalf of the entire Board to those directly and indirectly affected by recent events – “especially those service users, their families and carers treated so poorly at the Edenfield Centre.”
October 2022
GMMH further breaches human rights of patients imposing a blanket ban on personal mobile phones for in patients at Edenfield
It has come to CHARM’s attention that the management at Edenfield have removed mobile phones from all patients on wards at the Edenfield site, As of 13 October. We believe a blanket ban of this nature is a breach of Article 8 of the European Human Rights Convention. The right to a private and family life.
Such practices also create environments that further alienate patients from the outside world. This is not a route to recovery. The failings at Edenfield happened because there was a lack of oversight and openness. When a ‘behind closed doors’ culture of secrecy is implemented, it makes abuse more likely to happen. Meanwhile, workers have been allowed to keep their phones. This is unfair.
‘Treated worse than animals’: Huntercombe investigation reveals decade of mistreatment in care of more than 20 teenagers
A Sky News investigation into five hospitals run by The Huntercombe Group has revealed repeated allegations of over-restraint and inadequate staffing, which youngsters say left people at increased risk of self-harm
More than 20 former patients or their relatives have revealed how they were “treated worse than animals” and failed by the “awful” care they received at mental health hospitals for teenagers.
Testimonies gathered in an investigation by Sky News raise repeated allegations of over-restraint and inadequate staffing which youngsters say left people at increased risk of self-harm.
Rowan Thompson: Inquest into the death of teen mental health inpatient concludes neglect
The inquest into the death of teenager Rowan Thompson concluded on the 31 October 2022), with the jury finding that Rowan died of Cardiac Arrythmia due to Severe Hypokalaemia of unknown cause, contributed to by neglect due to the failure to communicate the findings of blood tests.
The inquest was heard over six days at North Manchester Coroner’s Court in front of HM Senior Coroner Ms Joanne Kearsley, sitting with a jury.
Rowan died on 3 October 2020 whilst an inpatient at the Gardener Unit, a medium secure adolescent mental health unit in Prestwich run by Greater Manchester Mental Health NHS Foundation Trust (GMMH). Rowan, who identified as non-binary, was 18 at the time of their death.
Prestwich unit bosses can’t check CCTV despite ‘five workers failing to observe patients’ the day teenager died, inquest hears
Bosses cannot check workers on a Prestwich mental health unit are carrying out observations using CCTV, despite five staff failing to do so correctly the day a teenager died, an inquest has heard. Rowan Thompson died aged 18 on October 3, 2020.
The teenager, who identified as non-binary and used the pronoun ‘them’, was an inpatient on the Gardener Unit, run by Greater Manchester Mental Health NHS Foundation Trust (GMMH), on the site commonly known as Prestwich Hospital. Rowan’s inquest previously heard they were supposed to be observed every 15 minutes, but staff did not check on them for 90 minutes before they were found having a seizure.
At Rochdale Coroners’ Court this morning (Thursday, October 27), the inquest heard that five members of staff working on-site that day had either wrongly signed records of observation or failed to carry out the duty. Rachel Green, head of operations for children and adolescent mental health services (CAMHS) for GMMH at the time, told jurors she was working in an adjacent building to the Gardener Unit on the day of Rowan’s death.
She told the court that no staffing issues had been brought to her attention before the tragedy unfolded, and that she had not visited the Gardener Unit herself that day until emergency services were in attendance. It was the following day that Ms Green discovered staff had not carried out the checks as they had claimed.
Edenfield Centre: Health minister backs public inquiry over abuse
The mistreatment of patients at a mental health hospital does warrant a public inquiry, a health minister has said. Will Quince apologised to patients at the Edenfield Centre in Prestwich near Manchester and their families.
A BBC Panorama investigation found a “toxic culture of humiliation, verbal abuse and bullying” at the hospital. Hospital bosses said they took immediate action including suspending staff and launching a clinical review.
Raising the case in the House of Commons, Bury South MP Christian Wakeford said it had been 15 days since the Panorama show aired “deeply distressing” scenes at the hospital, which had “brought tears across the country”, yet “we have heard nothing from the department”.
Manchester Council calls for public inquiry into mental health unit at centre of BBC Panorama investigation
Manchester City Council will ask the government for a public inquiry into a mental health unit at the centre of a BBC Panorama investigation earlier this year.
Undercover footage of the Edenfield Centre in Prestwich included allegations of inappropriate and neglectful behaviour, a toxic staff culture and poor care.
Andrew Maloney, deputy chief executive of Greater Manchester Mental Health (GMMH) NHS Foundation Trust which runs the centre, told councillors at a health scrutiny meeting on Wednesday (October 12) about the action taken in response.
However, the health scrutiny committee was not satisfied with this, describing the situation as a “catastrophic disaster”.
Demands for public inquiry amid ‘catastrophic disaster’ at mental health unit
Manchester council will ask the government for a public inquiry into a mental health unit at the heart of a BBC Panorama investigation aired last month. The calls for an inquiry come with fears that alleged abuse of patients at the Edenfield Centre, as claimed by the BBC, is happening at other Greater Manchester’s mental health treatment units.
Staff, including support workers, and registered nurses, were secretly filmed by an undercover Panorama reporter embedded in the unit from March to June of this year. The footage appeared to show patients being bullied, humiliated, swore at, and taunted.
Edenfield Centre: Care watchdog praised bosses at abuse hospital
The healthcare watchdog praised bosses of a mental health hospital after visiting during the weeks when the BBC filmed patients being mistreated.
According to a report to governors at the trust which runs the Edenfield Centre, the Care Quality Commission noted its “strong, motivated leaders”.
After the BBC gave it information about the abuse, the watchdog suspended the hospital’s “good” rating.
The CQC said it would take further action if needed.
University of Salford removes student nurses from NHS mental health unit under investigation by police
A University has withdrawn its student nurses from a mental health unit which is under investigation by police. The Edenfield Centre in the grounds of the former Prestwich Hospital in Bury is the focus of a criminal investigation after allegations that patients were abused.
Now the University of Salford has taken action in the wake of the allegations. A University of Salford spokesperson said: “Greater Manchester Mental Health NHS Foundation Trust (GMMH) provides placements for a number of universities and across professions. All of our students who were on placement or due to attend placement at the Edenfield Centre are now being moved to alternatives. The wellbeing of our students is our top priority, and we have been in touch with all affected students to offer support.”
The Edenfield Centre: Bereaved family ‘reeling with anger’ at abuse
Relatives of a woman who died at a mental health unit where a culture of abuse and mistreatment was uncovered say they have been left “reeling with anger”.
A BBC investigation found evidence of routine humiliation and bullying at the Edenfield Centre in Manchester.
Hospital bosses said they took immediate action to protect patients.
But the sisters of one patient, who died in 2017, said they had “little confidence” improvements would be made.
September 2022
The Equality and Human Rights Commission response to allegations about mistreatment of people in Edenfield Centre Mental Health Unit
The Equality and Human Rights Commission has a duty to enforce equality laws and defend human rights. We therefore consider all allegations of unlawful activities carefully and take action where necessary.
Responding to allegations shown by BBC Panorama on 28 September about the treatment of people in Edenfield Centre Mental Health Unit, in Prestwich, the Chief Executive of the Equality and Human Rights Commission, Marcial Boo, said:
“The reports of potentially unlawful activity at the Edenfield Centre Mental Health Unit in Prestwich may indicate a breach of patients’ human rights. These include the right of patients to be free from inhuman and degrading treatment, their right to liberty and security and their right to private and family life, including physical and psychological integrity.
‘Lessons will be learned’? Responding to Panorama’s documentary on abuses at the Edenfield Centre
It should never require a television documentary to shock a society into acting on institutional abuses in any public service, let alone those treating people who are at their most vulnerable and traumatised. Yet sadly it too often does. This week’s Panorama programme exposing serious abuses at the medium secure Edenfield Centre in Greater Manchester joins a litany of similar programmes that have forced the public to confront the consequences of a failure to provide care that meets basic standards of human decency.
The programme was distressing viewing for anyone. For some, it will have opened their eyes to abuse that has been happening in institutions for as long as they have been a part of our mental health care system. For people living with a mental health difficulty and their families, it will have been unimaginably traumatic to witness this abusive treatment; while for some it will be all too painfully reminiscent of their own experiences.
We need to ask why this continues to happen in our NHS in 2022.
‘Toxic culture’ of abuse at GMMH mental health hospital revealed by BBC secret filming
Humiliated, abused and isolated for weeks – patients were put at risk due to a “toxic culture” at one of the UK’s biggest mental health hospitals, BBC Panorama can reveal.
An undercover reporter at the Edenfield Centre filmed staff using restraint inappropriately and patients enduring long seclusions in small, bare rooms.
Staff swore at patients and were seen slapping or pinching them on occasion.
Hospital bosses said they have taken immediate action to protect patients.
Greater Manchester Mental Health NHS Foundation Trust, which runs the medium secure unit, said it was taking the allegations “very seriously”.
A number of staff members have been suspended, and the trust said it was working with Greater Manchester Police, the independent healthcare regulator the Care Quality Commission, and NHS England “to ensure the safety of these services”.
Greater Manchester Police said it has opened a criminal investigation.
Shocked and concerned’ – Mind calls for a public inquiry after BBC Panorama exposes alleged verbal and physical abuse of patients at Edenfield Centre
Undercover footage broadcast during a BBC Panorama programme which aired yesterday evening highlighted alleged verbal and physical abuse of vulnerable patients with mental health problems and autism at the Edenfield Centre, run by Greater Manchester Mental Health NHS Foundation Trust. The programme raised serious concerns about the use of harmful and dangerous practices including unnecessary restraint and seclusion, near-mistakes with medication, falsification of observation records and physical and verbal abuse.
As a result, mental health charity Mind is calling for a full statutory public inquiry into systemic failings of inpatient mental health services across England.
Responding to the documentary, Vicki Nash, Associate Director of Policy, Campaigns and Public Affairs at Mind, said:
“The footage of patients at the Edenfield Centre obtained undercover by BBC Panorama is shocking and extremely concerning. People who have been admitted to medium secure units are likely to be experiencing moderate to severe mental health problems including suicidal thoughts, self-harming and psychosis. When we are at our most unwell and vulnerable, we need caring and compassionate treatment in a safe and therapeutic environment to recover and we and our loved ones should be able to expect – as a bare minimum – basic humanity and respect. The fact that footage obtained as part of this documentary has prompted a criminal police investigation indicates just how short of expectations this mental health service may have fallen.
“We are especially concerned about the apparently excessive and punitive use of restraint and seclusion for people with mental health problems and autism. We know these dangerous measures are traumatising, likely to make people’s mental health even worse, and can even be fatal – either directly or indirectly.
The Edenfield Centre: MP criticises mental health unit bosses over abuse
An MP has condemned the “horrific” treatment of patients at one of the UK’s largest mental health hospitals.
A BBC Panorama investigation found a “toxic culture of humiliation, verbal abuse and bullying” at the Edenfield Centre in Prestwich near Manchester.
Bury South MP Christian Wakeford said it showed a “failure of leadership” at Greater Manchester Mental Health NHS Foundation Trust (GMMH).
Nurses investigated amid abuse at Manchester mental health hospital
Nurses working at the mental health unit in Manchester are to be investigated by the regulator, after footage of vulnerable patients being subjected to humiliation, verbal abuse and bullying at the hospital was aired on the BBC programme Panorama.
Nurses and other staff at Edenfield Centre, which is a large medium security mental health unit in Prestwich, Greater Manchester, were filmed mistreating patients by an undercover BBC reporter working as a support worker at the centre, as part of a Panorama investigation.
“We’ve opened fitness to practise cases for some professionals on our register”
Andrea Sutcliffe
Staff, including mental health nurses, were filmed mocking patients when they were in vulnerable situations, and joking about their self-harm.
In addition, they were seen using unnecessary restraint and slapping or pinching patients. They were also seen keeping patients with autism or learning disabilities in seclusion for long periods of time.
What is behind a new mental health abuse scandal?
Edenfield treats around 200 patients, most of which have been sectioned by a court and are classed as a potential danger to themselves and others. The BBC’s footage from there is said to be as harrowing and shocking as that taken at Winterbourne.
It will almost certainly lead to outrage that health professionals could treat some of the most vulnerable people in society in such a terrible way. But mental health workers elsewhere in Britain have told Socialist Worker that what happened at Winterbourne, and now seemingly Edenfield is not simply the result of cruel and sadistic people in the workforce.
“People going to work in secure settings need to be extremely qualified and experienced,” one mental health practitioner told Socialist Worker on condition of anonymity.
“Patient behaviour can at times be very challenging, and even violent. But too often I hear that secure wards and units are staffed by people with little experience, and sometimes not a single registered nurse on shift.
“That is a recipe for disaster. If you don’t have enough experienced and skilled staff on, there is nobody to ensure a proper culture of care or to help with patients that are particularly distressed. Even very good staff without qualifications and practice simply don’t have the weight to do this.”
CQC suspends GMMH rating for Forensic inpatient or secure wards as a result of concerns about this service.
Greater Manchester Mental Health Trust suspends staff after alleged mistreatment of patients in mental health unit
Footage obtained by Panorama of the alleged mistreatment is harrowing. The programme is scheduled to be broadcast on Wednesday next week.
An NHS trust has suspended staff after allegations that patients were mistreated at a mental health unit. Last week it was revealed police are preparing to investigate the claims which relate to the Edenfield Centre based in the grounds of the former Prestwich Hospital in Bury.
The unit cares for adult patients. The Manchester Evening News understands that action was taken after the BBC Panorama programme embedded a reporter undercover in the unit and then presented the NHS Trust which runs it with their evidence.
The Edenfield Centre has 11 wards and it is understood staff working on both male and female wards have been suspended. Meanwhile GMP are continuing to assess evidence in relation to the allegations.
Manchester City braced for ‘Winterbourne View’-level scandal
Well-placed sources have now told Health Service Journal the allegations include “serious abuse” of adult patients, which they said were at a “similar sort of level as Winterbourne View”. The sources said the trust has already suspended a number of staff, although the trust refused to confirm this had happened.
The documentary has yet to be aired, but police are also aware of the allegations and are preparing to open an investigation.
Police prepare for investigation into The Edenfield Regional Secure Unit following alleged mistreatment of patients by BBC Panorama programme
The Edenfield Centre is a secure unit helping mental health patients adjust back into the community. It works mainly with people who have been in prison or admitted to hospital following a criminal offence.
The Edenfield Centre based in the grounds of the former Prestwich Hospital in Bury is at the centre of the claims.
The unit cares for adult patients. The Manchester Evening News understands that action was taken after the BBC Panorama programme embedded a reporter undercover in the unit and then presented the NHS Trust which runs it with their evidence.
A spokesperson for GMP said: “We are aware of the allegations and are liaising with partner agencies to safeguard vulnerable individuals and obtain all information required to open an investigation.”
A spokesperson for Greater Manchester Mental Health NHS Foundation Trust said: “We can confirm that BBC Panorama has contacted the Trust, following research it conducted into the Edenfield Centre. We would like to reassure patients, carers, staff, and the public that we are taking the matters raised by the BBC very seriously.
Mental health hospital in Bury where patients were ‘bullied and abused by staff’ put into special measures
A report found staff ‘could be patronising, antagonistic, rude and made negative comments about patients’
A hospital where patients say they were ‘bullied and abused by staff’ has been placed into special measures. Cygnet Bury Hudson has been ordered to improve safety after its overall performance was judged to be ‘inadequate’, following an inspection by the Care Quality Commission (CQC) in June.
The hospital, off Bolton Road in Bury, provides low and medium secure inpatient mental health services for men and women across six wards and 78 beds. The service was last inspected in July 2020 when it was registered as Cygnet Bury.
Since April 2021, the location has been split into three and this is the first inspection at this location. During the recent visit, inspectors say patients told them they were being ‘bullied and abused by their peers and staff members’ and that they did not feel safe on wards.
A damning report published today reveals there were also issues with safeguarding, complaint handling, medicines management and staff attitudes to patients and carers.
Staff at women’s mental health facility ‘fell asleep’ when they were meant to be observing high-risk patients
Eleanor Independent Hospital in West Didsbury has been placed into special measures
A women’s mental health facility in south Manchester has been put into special measures after members of staff were found to have fallen asleep when they were supposed to be monitoring high-risk patients.
Eleanor Independent Hospital in West Didsbury was rated ‘inadequate’ following an inspection by the Care Quality Commission (CQC) in May – which also found some staff didn’t know the names of patients they were caring for.
The hospital, run by Eleanor EHC Limited, provides care for up to 34 women who have been diagnosed with a personality disorder or mental illness. The service was previously rated as ‘requires improvement’ following an inspection in 2021.
Inspectors highlighted significant concerns about the medicines management at the hospital and found errors around the prescribing, recording, and dispensing of medicines which placed people at a serious risk of harm.
“Patients and their carers reported that staff weren’t very caring and didn’t seem to be fully aware of how to support the people in their care. Staff were often on their phones instead of supporting and engaging with people,” they said.
Anger after GMMH Trust says it has no plans to publish ‘independent’ review into to deaths of three young people
“We want to know what it says and the wider public has a right to know.”
Families have blasted a NHS Trust after it said it did not intend to publish an independent review into their loved ones deaths. Three young people died in nine months at the same mental health unit.
A Coroner was told last week that the review will be “ready” this month. Rowan Thompson, 18, died while a patient at the unit, based in the former Prestwich Hospital, Bury, in October 2020, followed by Charlie Millers, 17, in December that year, and Ania Sohail, 21, in June last year.
Earlier this year, Greater Manchester Mental Health NHS Foundation Trust (GMMH), which runs the hospital, commissioned an ‘external report’ into the deaths. On Tuesday last week a pre-inquest hearing into the death of Rowan – who used the pronoun ‘they’ – heard that the full report would be available for the coroner to read ‘on or around September 30’
Trust ordered to produce report after deaths of three patients at Prestwich Hospital
Asked by the Manchester Evening News if the review would be published a spokesperson for the Trust said the Trust “always act on the wishes of the family regarding publication of reports,” adding “and so in line with this we have no immediate plans to make the report public.”
August 2022
July 2022
Prestwich Hospital mental health service’s safety rated ‘inadequate’
An NHS Trust based in Prestwich does not have enough staff to keep patients safe according to an independent review by the health and social care watchdog.
The Care Quality Commission (CQC) conducted a focused inspection of Greater Manchester NHS Mental Health Foundation Trust’s adult mental health services in April.
The inspection was carried out at the trust, based at Prestwich Hospital, after the CQC received concerning information about the safety and quality of the services provided.
The inspection reviewed the safety of the trusts’s community-based mental health services of adults of working age in April and concluded the service’s provision in this area was “inadequate”.
The inspection concluded safety standards at the service had deteriorated after a previous inspection of community-based mental health services for adults in 2019, which gave safety in this area a rating of “requires improvement”.
Safety is one five areas in which services can be assessed, and the trust currently holds an overall rating of “good” in every area except its safety.
The CQC’s report, published in June, says “the service did not have enough care coordinators and support staff to keep patients safe.”
June 2022
The mental health and dementia hospital where staff ‘didn’t know patients’ names’ and ‘told them to sit down whenever they tried to get up’
A mental health care hospital has been shut down by watchdogs after investigators uncovered shocking practices. The care unit was slammed for staff ‘not respecting the privacy and dignity’ of patients, as ‘staff often talked over patients, ignored patients, and talked about their personal hygiene needs in the main lounge’, while ‘patients were told to sit down whenever they tried to get up
Monet Lodge in Withington, Manchester, run by Making Space, provided care for up to 20 older people with complex mental health problems, specialising in dementia care. After the damming inspection in early March of this year, the location was barred from admitting any further patients and instructed to discharge current patients, or find them new placements, by the end of that month.
Concerns were first raised by the Care Quality Commission (CQC), a social care watchdog back in February 2021, when Monet Lodge was placed into special measures. It found that the building was ‘not safe, unclean, not well equipped, not well furnished, not well maintained and unfit for purpose’, and that ‘staff had not received basic training to keep patients safe from avoidable harm’.
May 2022
Inquest for 19 year old who died in the Rivington Unit at at Royal Bolton Hospital in 2021
The inquest will ask if there were ‘missed opportunities’ in care of teen who died in mental health unit. Outlining the ‘scope’ of the inquest, Timothy Brennand, senior coroner for Manchester West, said it would consider three main areas: the care and treatment Grace received from Greater Manchester Mental Health Trust from January 2020 to her to death; the care and treatment she received while a patient at the Rivington Unit and the impact her autism and ADHD had on the treatment and risk assessments she received.
An inquest into the death of a teenager in a mental health unit will examine if there were any ‘missed opportunities’ in her care and treatment. Grace Victoria Heald, 19, of Blackley, died in the Rivington Unit at at Royal Bolton Hospital on August 22 last year.
Greater Manchester Mental Health Trust criticised after seven-year-old Emily Jones killed by patient
After Emily’s death, Greater Manchester Mental Health NHS Foundation Trust (GMMH) – who had been treating Skana – conducted an internal review and said it was “difficult to see how this incident could have been prevented”. But NHS England has now disagreed with GMMH’s assessment, saying there was not ‘sufficient analysis’ to justify their conclusion. Its own investigation found Skana, who has paranoid schizophrenia, was “potentially dangerous when unwell” and that “it was clear by 2017 that [she] presented risks to others when she was ill, but not when she was well.
Greater Manchester Mental Health Trust has been criticised by NHS England after Trust said it was difficult to see how it could have prevented the murder of a seven-year-old girl by one of its patients.
The report said: “Our most important finding is that the trust’s understanding of risk concepts was poor.”
April 2022
Autistic girl, 14, unlawfully detained in hospital, high court judge finds
The high court in London. Mr Justice MacDonald described the hospital environment into which the girl was placed as ‘brutal and abusive’. In his judgment, MacDonald refused to grant a request from Manchester City Council for the local authority to remain anonymous. He criticised the council for failing to find her a suitable placement throughout the month she was unlawfully detained in hospital, accusing the council and unnamed NHS trust of having “comprehensively failed in this case”.
A 14-year-old autistic girl was unlawfully detained in hospital and restrained in front of scared young patients, a high court judge has found.
Mental health team didn’t believe mum-of-one posed a ‘significant risk’ to herself days before train station death
Day two of the inquest in Stockport heard how doctors at the Bronte ward at Wythenshawe Hospital, where Kate was being treated after being sectioned under the Mental Health Act, felt her condition had improved enough for her to be discharged to the home based treatment team. This is despite earlier ‘manic behaviour’ on this ward and Kate going missing when granted unaccompanied leave.
Mental health practitioners did not believe a mum-of-one posed a ‘significant risk’ to herself in the days and weeks leading to her death, an inquest has heard. Kate Hedges, 35, passed away at Gatley train station in November 2020 having been released from hospital in October and referred to the home based treatment team.
Schoolgirl, 13, ‘did not intend to end her own life’, coroner rules
Faith Hindle, from Salford, killed herself a day after telling an “overburned” mental health nurse that she feared she was unable to keep herself safe. She was pronounced dead at Royal Manchester Children’s Hospital after being found hanged at her family’s home in Cadishead on the evening of December 8, 2018.
At an inquest at Bolton Coroner’s Court today, a coroner ruled that Faith, a pupil at Irlam and Cadishead Sports College, died as a result of “misadventure”. The hearing was told that in the months prior to her death, Faith’s family, school and GP practice had tried to help her access mental health support after she began self-harming.
In August 2018, two referrals were made to Salford Children and Adolescent Mental Health Service (CAMHS) after Faith attempted suicide, the inquest heard. Tayaba Nicholson, a mental health practitioner at Salford CAMHS, picked up the referral and promised to see Faith on a “three to four week basis”.
‘Special’ son, 22, died after ‘never getting over’ his counsellor using gravestone reference in therapy
A counsellor apologised to a client after using imagery of ‘a gravestone’ in a therapy session, a court heard today. Benjamin Davis then took his own life only a few months later, having ‘never got over that experience’, his father said.
During an inquest in Bolton today (April 13), private counsellor Avremi Rosenberg admitted that he should have used different wording in his session with Benjamin, who was 21 at the time. He also accepted that the language was ‘inappropriate’.
he youngster was also diagnosed with autism in 2021, assistant coroner Rachel Syed heard. After this diagnosis, Benjamin had five counselling sessions with Mr Rosenberg in spring last year.
And it was during these sessions in which Mr Rosenberg referenced a gravestone, Mr Davis said. He added: “I asked Mr Rosenberg about it and he confirmed he did [say it].
“My son is autistic and he cannot process things in the way other people do. If you mention a gravestone to me, it is okay, but if you mention it to autistic people they will focus on the picture of the gravestone.
“You have to be careful with language… they take things very literally. He told me that he started to think about death again after that. He never got over that experience. He was in a good place with autistic acceptance.”
When asked why used the imagery, Mr Rosenberg said he said ‘in the context that his autism diagnosis was… part of him but not all of him’. He added: “Benjamin approached me because he knew I was a counsellor with experience with working with people on the autism spectrum. In hindsight, this would have been better dealt with by the NHS. I did apologise to Benjamin for the way it came over.
March 2022
Mother’s agony after suicidal daughter escapes from GMMH hospital despite being sectioned
A worried mother says her suicidal daughter escaped from a mental health hospital on numerous occasions. The woman says her 21-year-old daughter, whose names are being withheld to protect their identity, was sectioned under the Mental Health Act and admitted to Griffin Ward at Prestwich Hospital ten months ago.
The mother, who lives in Collyhurst, says her daughter’s mental health suffered terribly after her (the mother’s) father died four years ago, and then further declined when she was attacked by two girls in Piccadilly Gardens in Manchester last June.
She says her daughter was sectioned immediately after a member of public alerted police after seeing her stood on a bridge.
After attempting to take her own life, she spent a few days at Salford Royal and Park House before being transferred to the Griffin Ward at Prestwich Hospital. But she says her daughter has been able to escape from the hospital on several occasions and has further attempted to take her life each time.
Mental health service failings possibly contributed to dad killing his baby son, coroner says
A coroner has delivered a damning condemnation of the mental health treatment of a psychotic man in the months before he threw his 11-month-old son into a river and to his death.
The failures leading up to the horrific events which claimed the life of Zakari William Bennett-Eko on September 11, 2019, represented an ‘arguable breach’ of Article 2 of the Human Rights Act , which says government organisations have a fundamental legal duty to protect life, the Rochdale inquest was told.
Kelly Darlington, solicitor for Emma, said “This is an extremely distressing case that no mother should ever have to experience.
“The inquest into the death of Baby Zakari highlighted a number of multi-agency failings in the care of his father who was experiencing a serious relapse of his psychosis at the time of the horrific events that led to his death.
“These missed opportunities may have avoided the serious deterioration in the father’s mental health that led to the unlawful killing of Baby Zakari.”
Eight organisations and baby Zak’s mum were legally represented at the inquest. The organisations were: Greater Manchester Mental Health Trust, Manchester City Council, Bury Borough Council, Manchester Clinical Commissioning Group, Manchester Foundation NHS Trust, Pennine Care NHS Foundation Trust, Mersey Care NHS Foundation Trust, Rock Health Centre and Greater Manchester Police.
Ms Kearsley has given legal representatives of all eight organisations 28 days to prepare submissions in advance of a ‘Regulation 28 Prevention of Future Deaths’ report.
The report will be sent to authorities which have the power to make the changes that are suggested. Organisations have to respond to these within 56 days showing how they have made changes according to the coroner’s recommendations, or how they intend to. All Prevention of Future Death reports and responses are sent to the Chief Coroner.
Man discharged from MRI mental health unit died hours later after trying to take own life outside
Daniel Kirton may have had his ‘right to life’ breached, a pre-inquest review heard today.
A man who died after trying to take his own life inside hospital grounds just hours after being discharged from its mental health unit could have had his ‘right to life’ breached, an inquest heard.
Daniel Kirton, 35, visited the mental health team at Manchester Royal Infirmary on December 3, 2020, before he was discharged.
Tragically, though, after he left he tried to take his own life on hospital grounds, before ‘rolling’ onto nearby Upper Brook Street. He was hit by a taxi at around 11.35pm and pronounced dead in the hospital on December 4.
Family will have to wait for answers over son’s death at GMMH mental health unit
Charlie Millers was one of three young people to die at Prestwich Hospital over a nine-month period. Greater Manchester Mental Health NHS Foundation Trust (GMMH), who run the site, have been ordered to commission an “external report” about all three deaths by NHS England. A pre-inquest review held at Rochdale Coroner’s Court today, March 8, heard that the inquest into Charlie’s death could be delayed by “several months” due to this report.
An inquest into the death of a teenager being treated at a mental health unit in Prestwich will be delayed “several months” after the NHS trust in charge was ordered to produce a report into the incident.
Anti-psychotic drugs contributed to death of man with mental health history, inquest hears
A man died after a build up of side effects from a drug he was taking to treat his paranoid schizophrenia led to his organs failing, an inquest heard.
John Warren had battled mental health problems since his early 20s. He was diagnosed with paranoid schizophrenia in 1988, a jury at Manchester coroners court heard.
He was moved to the Priory psychiatric hospital at Cheadle Royal hospital in 2000, where he had been ever since.
Tragically, though, side-effects from a drug – clozapine – caused internal problems and, after he was not able to have surgery at Wythenshawe Hospital, he died a few days later.
February 2022
New £3m model of mental health support agreed in Salford
A new citywide mental health service has been approved, anticipated to support an additional 5,000 people per year in Salford.
‘Living Well Salford’, jointly funded by NHS Salford Clinical Commissioning Group (CCG), Greater Manchester Mental Health Foundation Trust (GMMH) and Salford Primary Care Networks, is the name given to the new local system designed to meet the needs of adults with mental health problems that require more support than primary care can offer, but don’t meet the criteria for secondary care mental health services.
January 2022
Sam Millers and Marc Thompson want answers after both their teenagers were admitted to Prestwich Hospital and didn’t come back out alive
The parents of two children who died in hospital due to “observation failings” are demanding an independent investigation.
Sam Millers and Marc Thompson are parents from two different parts of the county who both lost their children after they received treatment at Prestwich Hospital.
Sam, from Old Trafford, lost her trans son Charlie, 17, in December 2020 after “observation failings” led to his suicide.
Meanwhile the death of Marc’s son, Rowan, 18, who identified as non-binary, two months later still remains a mystery.
Their children make up two of three young people who have died while being admitted at Prestwich Hospital over the course of nine months, and are now demanding answers.
December 2021
Union fears ‘dangerous’ low staffing levels at Greater Manchester Mental Health Trust are harming patients
As reported in the Manchester Evening News last week a watchdog is “very concerned” about the safety of people using the services of Greater Manchester Mental Health NHS Trust.
A damning report said inspectors found there were not always enough nurses and that permanent staff did not feel safe if bank or agency workers were used as they didn’t have the relevant training.
It follows an unannounced inspection in September by the Care Quality Commission “due to on-going concerns about the safety of services”.
Now UNISON says it is concerned about “dangerous” staffing levels across the Trust’s sites in Prestwich, Trafford, Manchester, Wigan, and Bolton.
A Unison spokesperson said: “Our members have reported across the Trust that staffing levels are at dangerous levels and that this is impacting both upon patient care and staff well-being.
“Some of our members within the Early Intervention Service have recently voted for strike action over Trust re-organisation plans which would leave their service even more stretched.”
Unison North West regional organiser, Lyndsey Marchant, added: “Staffing levels are causing problems throughout the Trust. Recent reports about Prestwich Hospital were incredibly worrying, but UNISON is also concerned about issues within our community mental health services.
“Community mental health services do vital preventative work, which can often avoid young people from people admitted to facilities like Prestwich Hospital.
November 2021
Cheadle Royal Psychiatric hospital ordered to improve after failing to provide ‘caring environment’ for patients
Cheadle Royal psychiatric hospital has been ordered to improve after a watchdog found it was failing to provide ‘a caring environment’ that respected patients’ dignity and helped them recover.
Cheadle Royal Hospital, in Heald Green, has in-patient wards for adults and children as well as specialist eating disorder services.
It was previously rated ‘good’ overall by the Care Quality Commission (CQC) at its last full inspection in 2017.
The service has now been downgraded to ‘requires improvement’ after officials identified a ‘number of concerns’ at a visit earlier this year.
This is despite the watchdog noting that ‘staff treated patients with compassion and kindness’ and ‘developed holistic, recovery-oriented care plans’.
The Priory Group, which runs the hospital, says it is ‘working hard to make the improvements identified’ by the CQC.
During the visit, safety was found to be ‘inadequate’ in the acute adult wards and psychiatric intensive care units, as well as on the child and adolescent mental health wards.
A newly published report notes that ‘not all wards were safe, clean, well equipped, well furnished, well maintained and fit for purpose’.
Man charged with attempted murder after patient stabbed at mental health unit
A man has been charged with attempted murder after a patient was stabbed in the mental health unit of a hospital.
Police rushed to reports of a stabbing on October 27 at Park House, which contains adult inpatient mental health wards on the North Manchester General Hospital site.
A man in his 30s suffered serious injuries and had to be treated at the scene before paramedics could rush him to hospital for further aid.
An ambulance, air ambulance and a paramedic in a response vehicle all attended the scene.
A man, also in his 30s, has now been charged with attempted murder, officers have confirmed.
The incident is under both a criminal investigation, according to the force and the trust which runs the unit.
A spokesperson for Greater Manchester Police has said: “Police were called shortly after midday (Wednesday 27 October) to a report of a stabbing at Park House, Manchester.
“A man in his 30s suffered serious injuries but is now in a stable condition.
“A second man in his 30s has been charged with attempted murder.
“This was believed to be a contained incident and GMP are working with staff at North Manchester General Hospital to investigate the circumstances.”
October 2021
September 2021
‘Inadequate’ care home that failed to protect residents from potential harm or abuse placed in special measures
A care home that was failing to protect its residents from potential harm or abuse has been placed in special measures.
Smithy Bridge Court, in Littleborough, provides care for up to 51 people with complex care and mental health needs, including dementia.
But it has been rated as ‘inadequate’ by health watchdog the Care Quality Commission (CQC) following an inspection of the new-build facility in Barke Street.
READ MORE: Firm that provides at-home care for people with a range of health conditions failed to ensure staff were competent, watchdog says
This is the lowest grading a care home can receive and if ‘significant improvements’ are not made within six months it could potentially be closed down.
The inspection was prompted in part due to concerns raised over staffing levels, management of medicines and safeguarding.
Source: Manchester Evening News, 23rd September 2021
Legendary dance venue hosting huge mental health awareness event for pupils
The events programme has been designed by young people and was delivered in partnership with Manchester-based mental health charity 42nd Street.
Depot Mayfield played host (Thursday September 23) to 215 Greater Manchester schools and a series of live performances, workshops and lessons to explore the wellbeing and mental health challenges faced by young people – as well as the support available to them.
Source: Manchester Evening News, 23rd September 2021
Heartbroken mum learned of son’s death on Facebook
Mental health staff believed Kieron, who grew up in Withington, was regularly using drugs.
However, the court heard how Kieron denied any claims and was often “aggressive or agitated” when on the ward.
He was discharged in 2019 and offered a place with the housing association one year before his death.
Speaking at the inquest, Ms Hamlin, who had not seen her son in two years, said she didn’t find out about his passing until she read it in a Facebook post in September 2020.
During a toxicology report, pathologist Dr Justin Nkonge said Kieron’s lungs were found to be four times heavier than they should have been.
Blood tests showed there to be cocaine and heroin in his system when he died.
Kathyrn Dykes, clinical Psychologist for the Greater Manchester Mental Health NHS Foundation Trust, said a number of areas of expectation within the trust were not met during Kieron’s treatment.
She said this was because of the pandemic and face-to-face meetings not being possible.
Speaking at the inquest, she said: “Kieron would leave Hollybank very early in the morning and return at night, making it hard for mental health nurses to contact him.
“Notes had not been updated on the system due to workloads at the time.”
Ms Dykes said although Kieron had been placed in the “red zone”, meaning patients are in crisis, he should have been getting three visits a week.
Source: Manchester Evening News, 22nd September 2021
Call for ‘urgent review’ at Prestwich Hospital following death of teenager accused of murdering mother, coroner told
A campaign group has called for an ‘urgent review’ of Greater Manchester’s mental health trust following the death of a teenager at Prestwich Hospital, a coroner has heard.
Rowan Thompson, who used the pronoun ‘they’, was found dead at the Gardener Unit at the mental health hospital on October 3 last year.
Rebecca Titus-Cobb, a lawyer representing Rowan’s family, told the inquest the family had a number of concerns regarding Rowan’s treatment while on the unit.
She said there were ‘systemic issues regarding observation of patients on the unit’, and that the campaign group Inquest had contacted the Care Quality Commission to express concerns following a number of deaths, including Rowan’s.
She added: “The family understand that Rowan’s death was one of four recent deaths across Greater Manchester Mental Health Trust units, Junction 17 and the Gardener Unit where Rowan passed away.
“Clearly there are concerns about the general operation of the units. Inquest have requested that the Care Quality Commission undertake an urgent review and or inspection of the trust.
“In particular, the letter raised concerns that similar criticisms of Junction 17 were made at the previous inspection in February 2016 regarding incomplete observation records and missing entries.
“There are concerns that the issues in Rowan’s case may be part of wider, broader concerns that have arisen not only in Rowan’s case, but other cases.”
At the time of their death, Rowan was supposed to be under 15-minute observations, the court heard.
Ms Kearsley said the inquest would look into the observations practices on the day Rowan died.
Ms Kearsley ruled that scope of the inquest would include the care and treatment Rowan received at the hospital, as well as the observations by staff at the hospital on the day of their death.
An inquest had been scheduled for December, but is now likely to take place next year before a jury.
Source: Manchester Evening News, 23rd September 2021
Mental health patients leaving hospital in first lockdown felt lonely and isolated
Mental health patients who were discharged from or admitted to acute mental health services during the first Covid-19 lockdown experienced loneliness and social isolation, according to a new study.
Published in the journal British Journal of Psychiatry, the 34 patients, carers and clinical staff were interviewed by a team of researchers from The University of Manchester.
The study was funded by the National Institute for Health Research Greater Manchester Patient Safety Translational Research Centre (NIHR GMPSTRC).
NIHR GMPSTRC is a partnership between The University of Manchester and Salford Royal NHS Foundation Trust.
Mental health service users also reported ‘working harder’ to avoid admission due to fears around environmental safety as a result of COVID-19.
“Even before the pandemic, there are lots of safety concerns associated with recent discharge from inpatient mental health services, for example suicide and self-harm,“ said lead author Dr Natasha Tyler, researcher at the GM PSTRC and The University of Manchester.
Dr Tyler added: ‘Our patients and carers felt that because of the national need to free-up hospital beds, the quality of discharge and admission planning was compromised at times.
“That meant discharging patients from hospitals who were not ready to cope in the community or not admitting patients who needed in-patient care.“
Source: University of Manchester, 16th September 2021
Local businesses raise £60K for new community mental health initiative
A football-themed fundraising initiative, organised by Foundation 92 and Redstone Accountancy, has exceeded all expectations by raising £60,000 in donations from the Greater Manchester business community, to fund a new community mental health initiative.
A football-themed fundraising initiative, organised by Foundation 92 and Redstone Accountancy, has exceeded all expectations by raising £60,000 in donations from the Greater Manchester business community, to fund a new community mental health initiative.
Source: About Manchester, 16th September 2021
‘No mental health bed’: why children end up on acute medicine wards
Over the last five years there has been a gradual increase in the number of children admitted on to our acute paediatric unit who don’t need the kind of medical treatment we offer.
Consistently this summer, 20% of our beds have been occupied by children who need either a specialist mental health bed or a specialist residential placement in the community.
Not long ago we had a looked-after child of primary school age with serious behavioural issues who ended up stuck on our ward for several weeks because the local council couldn’t find them an appropriate placement in Greater Manchester. It was heartbreaking because they ended up 100 miles away, far from anyone they knew.
Many of these patients are not getting the care they need because neither I, my colleagues or the nursing staff are trained to provide the level of psychiatric care they require. We are trained to deal with medical problems. The mental healthcare teams don’t have the capacity to provide the level of daily input that these children need.
Source: The Guardian, 13th September 2021
Patient endured an 18-hour hour delay following a mental health call-out
Paramedics for North West Ambulance Service (NWAS) have told the Manchester Evening News that one patient endured an 18-hour hour delay following a mental health “Category 3” call-out.
90 pc of ‘Category 3’ calls should be responded two within two hours.
It comes amid reports of queues of ’14 ambulances’ outside Stepping Hill Hospital in Stockport.
Source: Manchester Evening News, 10th September 2021
“Unless similar units cease to receive public money, such lethal outcomes will persist” says independent report into deaths of adults with learning disabilities at hospital
“Unless similar units cease to receive public money, such lethal outcomes will persist” says independent report into deaths of adults with learning disabilities at hospital
An independent report into the deaths of King, Nicholas Briant, 33, and 36-year-old Joanna Bailey, who all died at Cawston Park, said their relatives described “indifferent and harmful hospital practices”.
The report, published on Thursday, makes reference to “excessive use of restraint and seclusion by unqualified staff” and a “high tolerance of inactivity”.
“Unless this hospital and similar units cease to receive public money, such lethal outcomes will persist,” the report said.
How many people from Greater Manchester are living in Units like this?
Source: The Guardian, 9th September 2021
August 2021
July 2021
Three young people have died at Prestwich mental health hospital in the last nine months
Three young people have died in a nine month period at Prestwich Hospital. Rowan Thompson, 18, died at the mental health hospital in Bury, in October, followed by Charlie Millers, 17, in December, and Ania Sohail, 21, in June.
The series of deaths has led campaigners to call on the Care Quality Commission to ‘urgently inspect the service’. In response, the Care Quality Commission told the Manchester Evening News they were reviewing ‘the information available to us and considering what actions’ to take. Paul Elliot, Deputy Chief Inspector for hospitals and lead for mental health said there were ‘areas for improvement’, adding: “We have made it clear that the trust needs to focus further on safety.
“In acute wards for working age adults and psychiatric intensive care units, staff were not following the trust’s policy in relation to rapid tranquilisation and in child and adolescent mental health wards, checks to ensure that equipment was safe to use had not always been carried out.”
Jodie Anderson, caseworker at the charity INQUEST, which is supporting the families of Charlie and Rowan, said they were ‘deeply concerned’.
“We await the inquests into these premature deaths, which must ensure the utmost scrutiny. However, we cannot wait for action on this hospital. In light of these three very recent deaths of young people in concerning circumstances, we call on the regulators the Care Quality Commission, to urgently inspect this service and ensure other young people in mental health crisis are kept safe.”
Click on title for full article.
Source: Manchester Evening News, 26th July 2021
Pennine Mental Health Trust failed young musician due to gap in provision
Self-taught drummer James Theophine was reported to the police in April 2019 and his mum Melanie Theophine said that the allegations ‘rocked his world’. James became dependent on alcohol and died from multi-organ failure in October 2020, aged 20.
The court heard that after his 19th birthday, James had struggled to access mental health services after getting too old for the children’s mental health team. He was considered ‘too complex’ for the adults’ community mental health team and was referred to an organisation called Lanc UK, which was commissioned to run some mental health services.
Lanc UK director Dr Neil Rutherford told court that his organisation had already considered that James was too complex for the organisation to help him one month earlier – an issue his mum had previously highlighted.
Ms Fletcher from Pennine Trust said she had not been made aware of that, and would have found an alternative solution for James had it known.
Asked whether she believed there had been a gap in provision for James, Ms Fletcher said: “Yes.”
Click on title for full article
Source: Manchester Evening News, 24th July 2021
High volumes of staff absences at GMMHT due to Covid-19 and poor communication between teams delayed help for Trauma Survivor who subsequently died

Attempts to reach Catherine and start work to help her reduce her drug intake were delayed as liaison staff believed she had been discharged, while home treatment staff believed she was still in hospital.
In addition, high volumes of staff absences due to Covid-19 gave way to long waiting lists for appointments also delayed Catherine being able to get help, said Michael Hartley, who led the report by GMMH’s governance body.
Click on title for full story.
Source: Manchester Evening News, 16th July 2021
GMMHT receives 30,000 calls to 24/7 Helpline since March 2020
At the start of the pandemic Greater Manchester Mental Health NHS Foundation Trust (GMMH) set up a 24/7, all-ages helpline within a week, staffed by experienced mental health practitioners from a range of services, many of whom were shielding themselves but supported to work from home.
In their first ten days, over 1,500 calls were received, and during the height of the pandemic the call handlers received almost 550 calls per day.
Since 20 March 2020, they have handled almost 30,000 calls and since its expansion in May, have supported the Greater Manchester Clinical Assessment Service (CAS) and NHS 111 service by streaming their calls and supporting the caller to a solution which helps relieve pressure on other services, including ambulance call outs and attendances at A&E.
Click on title for full story
Source: Rochdale News, 15th July 2021
Pennine Care sign staff health and wellbeing pledge
Pennine Care NHS Foundation Trust has become the latest NHS provider to sign a pledge supporting the principles of the Nursing Times Covid-19: Are You OK? campaign.
The trust signed up to support the campaign, after its Clare Parker, its executive director of nursing, responded to a call made by Nursing Times to NHS providers across the UK.
Pennine Care, which employs around 4,000 staff, provides mental health and learning disability services to people across Greater Manchester.
It runs a range of mental health and learning disability services for children and adults from sites in Bury, Oldham and Rochdale, Tameside and Glossop, and Stockport.
The trust highlighted that it had already taken a range of steps to protect staff mental health and wellbeing.
These include a dedicated staff wellbeing service offering support, counselling or therapy. Staff can self-refer or a referral can be made by a line manager.
Click on title for full article
Source: Nursing Times, July 2021
Young man, 22, began struggle with insomnia on holiday and was dead within months, inquest hears
David Marsden’s family slammed mental health care workers for his ‘dehumanising’ treatment on a ward at a hospital he once worked. Desperate mum Fiona tried to help her son as he was seen numerous times by his GP, A&E at Stepping Hill Hospital, as an outpatient with a psychiatrist and by the community mental health team.
Fiona slammed Norbury Ward, run by Pennine Care NHS Foundation Trust, during her testimony in court, saying through tears: “The ward environment was not what I or David expected. It added to his lack of self-worth.
“He was in hospital to be cared for, treated to get better. It was a place where he was secure and safe from harming himself. But there were occasions when I witnessed him being referred to as number B22, because for some care assistants it was easier to remember his room number than his name. On another occasion, I was sat with David and asked for a plain envelope which I knew they would have as there was an office on the ward. The care assistant looked down their nose and said no. David looked at me as if to say, ‘look, see’. The care assistant said ‘who are you?’ I replied that I was David’s mum and that I’d come to see him. “The care assistant said ‘oh, sorry, I thought you were one of the patients.’ This was the treatment that was supposed to help him get better.”
Click on title for full article
Source: Manchester Evening News, 13th July 2021
The £1.8m Salford project helping patients to leave hospital care because more than 40% don’t need to be there
Salford patients delayed on hospital wards are being helped to return to the community with a fresh start in a new home as part of a £1.8 million project.
Progressive landlord ForHousing has joined forces with Greater Manchester Mental Health NHS Foundation to tackle the long delays in people being discharged due to a lack of suitable properties.
A number of patients who have received mental health inpatient treatment in hospital or temporary mental health supported accommodation are affected and, according to NHS data, more than 40% of patients currently in mental health hospitals do not actually need to be there.
Click on title for full article
Source: Manchester Evening News, 9th July 2021
June 2021
Bed occupancy levels at Greater Manchester Mental Health Trust continue to exceed full capacity.”
Papers discussed by Greater Manchester Mental Health Trust’s board show that whilst demand for services dropped during the pandemic, community mental health services then saw a 26pc increase on pre-Covid levels in March – ‘suppressed demand that is now coming through’. Trafford clinical commissioning group noted a similar pattern.
Click on title for full article.
Source: Manchester Evening News, 27th June 2021
Man took his own life a month after mental health team said he was no longer an ‘urgent priority’
Steven Startup killed himself weeks after he was downgraded from an ‘urgent’ priority by a Greater Manchester Mental Health Trust mental health team. Stephen’s GP had referred him for desperate help after a chat about his suicidal thoughts but the nurse who did this assessment said it wasn’t likely he would act on it.
Click on title for full article
Source: Manchester Evening News, 24th June 2021
Death could have been prevented: Greater Manchester’s mental health trust ‘lost oversight
A heartbroken mum says she feels her daughter’s death could have been prevented if she had received the mental health treatment she desperately needed. Olivia Garvey was found ‘collapsed and unresponsive’ at the White Lodge Hotel, in Salford, last September – six months after her last involvement with mental health services.
Click on title for full article
Source: Manchester Evening News, 19th June 2021
Coroner will consider whether Greater Manchester Mental Health Trust could have done more to help a mother whose remains were found two years after she went missing
Inquest to be held because of questions over whether Greater Manchester Mental Health NHS Foundation Trust could have acted differently before Marie went missing. A coroner will consider whether GMMHT could have done more to help a mother whose remains were found two years after she went missing.The inquest will be heard at South Manchester Coroners Court, in Stockport, for five days from January 10, 2022. Representatives from Greater Manchester Mental Health NHS Foundation Trust will be among those giving evidence. The Coroner explained that the evidence he had seen had seen pointed to an ‘escalation of self harm’ in the run-up to Mrs Scott’s disappearance, and that there could have been opportunities to detain her which ‘could have been expected to avoid her death’.
Click on title for full article
Source: Manchester Evening News, 17th June 2021
Grandad desperate for help took his own life after being passed from ‘pillar to post’ by Greater Manchester Mental Health NHS Foundation Trust

Inquest heard man left ‘very upset’ when he learned from his GP, just a few days before he took his own life, that he had been discharged by the mental health team.
Manchester Evening News, 15th June 2021
Steven Myers, 49, from Wythenshawe, was found dead in room 222 at The Amblehurst Hotel in Sale on December 2 last year.
Previously homeless, he had been living in the ‘chaotic’ temporary hotel accommodation on Washway Road for eights months up until his death, the inquest heard.
An inquest into his death heard Mr Myers had been left ‘very upset’ when he learned from his GP, just a few days before he took his own life, that he had been discharged by the mental health team.
His GP referred him a second time but the inquest heard Greater Manchester’s mental health trust arranged an appointment for December 7, five days after his death.
Click on title for full article
Source: Manchester Evening News, 15th June 2021
May 2021
Woman had fatal heart attack due to years of taking antipsychotics, inquest hears
An inquest jury has identified a series of failings in medical services following the death of a woman suffering with mental health issues for nearly 20 years. The long-term side-effects of an antipsychotic drug given 58-year-old Elaine Mylchreest caused her to die of heart problems, the hearing at South Manchester Coroner’s Court in Stockport concluded.
The 11-member jury said that the medical cause of death was myocardial ischemia – which reduces the heart muscle’s ability to pump blood – and dilated cardiomyopathy, a condition in which the heart muscle becomes weakened and enlarged. Both of these symptoms were ‘probably’ caused by Elaine’s long-term use of Clozapine which had been prescribed as a result of a treatment-resistant mental illness and had proved beneficial in alleviating distressing symptoms for many years.
The jury pointed to ‘broader failings’ in the overall treatment by medical services of Elaine, but which did not contribute directly to her death. These included not carrying out an annual electrocardiagram (ECG) tests on Elaine which might have identified the heart problems sooner. They also highlighted issues in identifying the potential link between physical health and on ongoing Clozapine treatment. Coroner Christopher Morris said that Elaine died ‘as a consequence of a recognised complication of necessary medical treatment with Clozapine’.
Source: Manchester Evening News, 13th May 2021
April 2021
Mental health boss says it’s too much work to find out if legal consent has been given before administering controversial ECT Treatment
Dr Alice Seabourne, medical director at GMMH defends overuse of ECT in Greater Manchester saying it is in line with NICE guidelines. Dr Alice Seabourne disputes the findings of the recent Freedom of Information audit of the use of electroconvulsive therapy (ECT) that showed that GMMHT uses ECT at the fourth highest rate in the country,
Further, GMMHT did not answer all of the Freedom of Information questions it was asked especially about whether patients gave consent before the procedure. Her grounds for not providing the requested information was that it was not held centrally and finding it would ‘create an unreasonable amount of work’ especially considering the pressures of the pandemic.
Click on title for full article
Source: Manchester Evening News, 26th April 2021
Parents of man who killed himself after death of sister say he was ‘let down’ by GMMHT mental health services
Architecture graduate Stephen Thurm, 32, was found hanged in February 2020.
An inquest heard how Stephen had struggled with mental health problems in adolescence and this was ‘heightened’ after his sister was killed.
After the tragedy, the former Altrincham Grammar School and Nottingham University student, became isolated, attempted suicide and was sectioned on a number of occasions.
Assistant Coroner Chris Murray recorded a conclusion of suicide of suicide following a three day inquest at Stockport Coroners’ Court, on Wednesday (May 5). Mr Murray raised concerns about some aspects of Mr Thurm’s care and said he would be writing a ‘prevention of future deaths’ report.
The concerns included ‘inconsistencies’ in moving Mr Thurm in and out of the ‘red zone’ – a term used to describe increasing a patient’s contact with the care team in response to a deterioration in their mental health, a lack of time for care coordinators to complete notes, a lack of support Mr Thurm’s parents and concerns about how information provided by the family was used in care plans.
Mr Murray said: “There does not appear to be support for families in cases such as this.”
Source: Manchester Evening News, 6th May 2021
‘Shortcomings in care’ by Pennine Care NHS Foundation Trust found as man died after absconding from hospital amid ‘deteriorating mental health’
Senior Coroner to make report to the Department of Health and Greater Manchester Health & Social Care Partnership to prevent future deaths. At the time of Martin’s death, there was a failure to conduct a detailed risk assessment in the period while a bed was sought or to agree a joint plan to manage the risk. It is probable that failure contributed to his death.
Ms Mutch, the Senior Coroner told the court: “At the time of his death, there was a failure to conduct a detailed risk assessment in the period while a bed was sought or to agree a joint plan to manage the risk. “It is probable that failure contributed to his death.”
While Ms Mutch was presented with evidence to indicate that procedures and new documents had been implemented within the two trusts, including a clearer definition of how someone is deemed to be of ‘high risk’, she feared it was not enough on a ‘national’ level. As a result, Ms Mutch said she would be making a report to prevent future deaths directed to the Department of Health and Greater Manchester Health & Social Care Partnership.The senior coroner said the report would identify the need for a ‘documented risk assessment and a documented share care plan between acute and mental health trusts’. It would also look into the issues around mental health bed shortages and a ‘responsibility’ of care.
Ms Mutch explained: “There was a very clear message from all the mental health witnesses who gave evidence that the issues of beds are ongoing in terms of patients such as Mr Gibbons who need to be placed in those beds.
“Another issue is the fact that he was assessed by a mental health trust in that mental trust area but because he doesn’t live there, it’s another mental health trust that has to take responsibility for his care That’s not an issue with the trust, they’re following a system, but that’s something that clearly isn’t right.”
Source: Manchester Evening News, 23rd April 2021
‘Gross failings’ by Greater Manchester Mental Health Trust contributed to suicide of former rugby player inquest found
Within a crisis care plan compiled in February 2020, there was specific reference to expressions of concern on the part of the family being indicative of the deterioration of the deceased’s mental health. Such concerns were raised on April 16, May 7, September 17 and November 3.
Those concerns were not followed up by the care coordinator and as such there was no face-to-face review of the deceased; the family’s concerns were not escalated; the follow-up appointment for the CTO due in October 2020 was not arranged; the deceased’s care plan made no reference to the CTO or conditions; the deceased was not seen by a mental health professional after May 2020; for reasons unknown, neither the planned care coordinator contact on May 14 and November 24, nor any psychiatric review after April 9 took place; supervision was either inadequate or non-existent.
All of which amounted to gross failings and as such, sub-optimal care.
Source: Manchester Evening News, 23rd April 2021
March 2021
Pennine Care NHS Foundation Trust slammed after popular young artist survived jump from car park but killed himself in hospital
A jury has found mental services were ‘fundamentally flawed’ in their handling of a beloved son and brother who killed himself in a hospital ward and that a lack of communication between mental health teams, particularly after Ashley’s most recent admission, had partly contributed to his death.
Ashley’s family has criticised the mental health care their loved one received, saying that health care teams were ‘reactive instead of proactive’ and had a habit of ‘only intervening at the point they have to’ Brother Christopher also raised concerns that Ashley’s care ‘was too clinical’, adding that he felt medics ‘did not take the time to get to know’ their patient.
The jury found that the process of discharging him from the Rochdale hospital had been ‘wholly insufficient’ and that there had been a lack of documentation relating to his condition for medics to use. They also concluded that the ‘communication and handover documentation was fundamentally flawed’, and that this needed to be improved.
Coroner Lisa Judge said that she would likely have issued recommendations for change within the mental health services that cared for the young artist, but staff within the hospital had already undertaken a review and made changes.
“What is apparent is that, as a result of the root cause investigation, a formal document was prepared with recommendations that the authors had and all of those recommendations have been taken forward by the trust,” the coroner said.
Source: Manchester Evening News, 11th March 2021
February 2021
Father of Emily Jones hits out as review of GMMHT finds actions of patient that killed his daughter ‘could not have been predicted
Despite the evidence of previous violence towards others, threatening behaviour involving a child and the lack of medication monitoring, an internal GMMHT review concluded that the attack on Emily ‘could not have been predicted or prevented’.
Emily’s father, Mark Jones, has been heavily critical of the mental health services and has slammed review into Skana’s treatment. He says he is waiting for a second investigation, already announced by NHS England, which is set to be launched soon.
“It clearly highlights major failures in GMMH’s systems and a lack of communication,” Mr Jones said.
“The lack of communication was probably down to so many people being involved in Skana’s care. She was passed from pillar to post, and as a result, some clinicians were unaware of the threat she posed.
“The failings are clearly and comprehensively addressed in their review but they still continue to relinquish all responsibility for the actions that lead to my daughter’s death. I therefore welcome the further imminent review by NHS England. I await their findings and will act on it accordingly in due course.”
Source: Manchester Evening News, 8th February 2021
Melanie Hogben fell to her death from Arndale car park after battling mental health issues, inquest hears
Melanie, who leaves behind a son and a daughter, had been struggling with mental health issues for several years. She was sectioned under the Mental Health Act just months before her death after battling Schizoaffective disorder.
An inquest into her death at Manchester Coroners’ Court heard she was discharged from a mental health unit in June 2018.
Melanie was admitted to the Moorside Unit at Trafford General Hospital, which is run by the Greater Manchester Mental Health NHS Foundation Trust, on March 9, 2018.
During her admission, a consultant psychiatrist changed her medication to a depot injection for two weeks to ‘improve her symptoms’, the inquest heard.
Her partner Tony said they were ‘concerned’ by the injection because of the side effects she suffered.
By the time Melanie was discharged on June 13, her condition had improved and she was put back on her previous anti-psychotic medication.
She had regular visits from a care coordinator until the beginning of August, but wasn’t then seen or contacted by any mental health professionals until October 18.
That care coordinator went off sick before leaving her position, the inquest heard.
But despite being classed as ‘high-priority’ after being sectioned, Melanie wasn’t given a new care coordinator until August 22.
Her new coordinator Wilma Martin-Lawrence told the inquest she was on a two-week holiday at the time Melanie was added to her case load of 28 service users.
The inquest also heard how she was unable to work in her capacity as care coordinator on 21 out of 43 days at that time due to other professional commitments.
Ms Martin-Lawrence was unable to make contact with Melanie until the beginning of October after she had contacted mental health services to ask who her care coordinator was.
Melanie took her life just over two weeks later.
A serious incident review was carried out by the Greater Manchester Mental Health NHS Foundation Trust. It showed that there were ‘significant staffing issues’ at the time of Melanie’s death. Daniel Cottam, operational manager for mental health services in central Manchester, told the inquest the team ‘was under significant pressure at the time’.
Source: Manchester Evening News, 3rd February 2021
2020
December 2020
The tragic mistakes that sealed the fate of Zak Bennett-Eko
Zak Bennett-Eko killed his son and was found guilty of manslaughter by reason of diminished responsibility. The presiding judge at the Lowry Nightingale Court had one important question of his own – exactly how did it come to this?
There were some answers revealed in court, as three psychiatrists took to the witness box to try and make sense of the incomprehensible. They told a story of a severely mentally ill man – aware of his spiralling condition – ‘slipping through the net’ and being ‘failed by the system’ at every turn, to use the judge’s own words.
The judge addressed Bennett-Eko, though he was not present in court, as he sentenced him to a hospital order which would confine him to a secure prison hospital.
“The regular trips you made to A&E show that you made genuine and sustained attempts to seek professional help,” said Judge Fraser.
“You were trying, as best you could in this respect, and you expressly asked to be sectioned.
“Your difficulties in communicating would have made it a lot more difficult for doctors in a busy A&E department to recognise your mental state, and sadly, on each occasion you presented at the hospital the help you needed was not available.
“You have serious medical conditions requiring urgent, intensive and long-term treatment.
“However, it is not the only failure of the system in your case. You seem to have slipped through the net in terms of care for your mental illness, which with hindsight was far more serious than was realised at the time.”
Although the young dad came off his medication, it was clear he had enough insight to seek help when he felt his condition relapsing in the weeks before the killing. Altogether, Zak Bennett-Eko went to A&E six times in 2019, begging for help with his deteriorating mental health. On one occasion, he specifically asked medics to section him.
Source: Manchester Evening News, 22nd December 2020
